Abstract
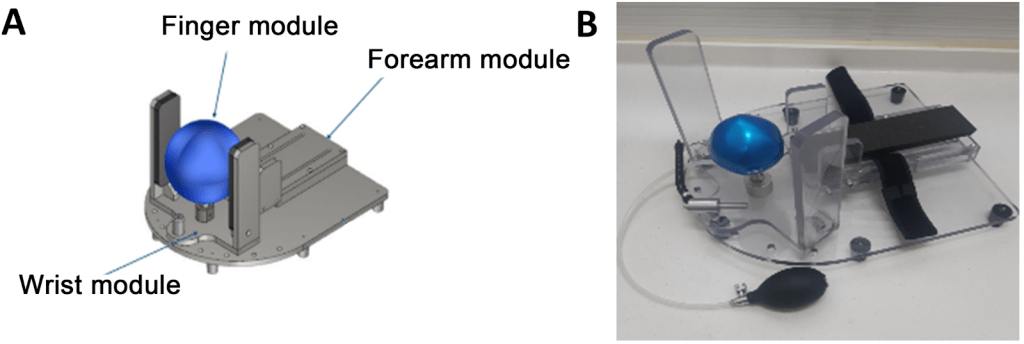
Spasticity is a common problem of central nervous system damage leaving functional impairment and problems related to the hygiene. We developed a straightforward stretching device for the wrist and hand. The device, primarily constructed from plastic, comprises a forearm support module, a wrist module, and a finger module. To assess the device’s effectiveness in managing spasticity among chronic stroke patients, twenty stroke patients used the device four times daily, 7 days a week, for 1 month. Spasticity severity was measured using the modified Ashworth scale (MAS) for the wrist, thumb, and index fingers. A questionnaire evaluated the device’s feasibility and areas for improvement. Before treatment, the mean MAS scores for the wrist, thumb, and index finger flexors were 1.50±0.36, 1.52±0.34, and 1.50±0.30, respectively, compared with 1.25±0.26, 1.27±0.30, and 1.32±0.33 post-intervention. Patients and occupational therapists expressed satisfaction with the device, citing its ease of use, effectiveness in stretching the wrist and fingers, and overall ease of manipulation. Half of the patients reported that all fingers were easily extended. The rigid plastic finger module was subsequently replaced with an inflatable, flexible rubber ball, providing a more comfortable contour for the stretched fingers, which increased user satisfaction. The stretching device effectively reduced spasticity in the wrist and hand, and the upgraded device enhanced patient satisfaction.
Keywords: Spasticity, stretching device, stroke, user feedback, pilot study
1. Introduction
Spasticity is a form of hypertonus characterized by increased muscle tension in response to stimuli,which intensifies with the velocity of joint movement1. It is a common sequela of central nervous system disorders, including stroke, traumatic brain injury, spinal cord injury, multiple sclerosis, and cerebral palsy. After a stroke, approximately 65% of patients experience spasticity2. This condition can lead to muscle tightness and joint stiffness in the affected extremity, resulting in functional disability3. Therefore, effective management of spasticity is crucial for stroke patients. Several methods are currently employed to manage spasticity in stroke patients, including oral medications, botulinum toxin or alcohol injections, bracing, serial casting, and stretching exercises4,5,6,7. Among these therapeutic options, stretching exercises, which involve moving joints through their full range of motion via an external force, are one of the most fundamental approaches8,9. However, stretching exercises are typically performed manually, requiring a therapist to administer repetitive exercises regularly10. This manual approach is time-consuming, and outcomes can vary depending on the therapist’s experience. To address these limitations, various stretching devices have been developed, demonstrating positive effects in reducing spasticity11,12,13. If patients could independently wear and use these stretching devices without the assistance of therapists, or with minimal help, it would save therapists’ time and enhance the effectiveness of spasticity management.
We developed a wrist and hand stretching device designed for patients to use conveniently. We evaluated its effectiveness and assessed feasibility through patient feedback, leading to subsequent device upgrades based on this feedback.
2. Results
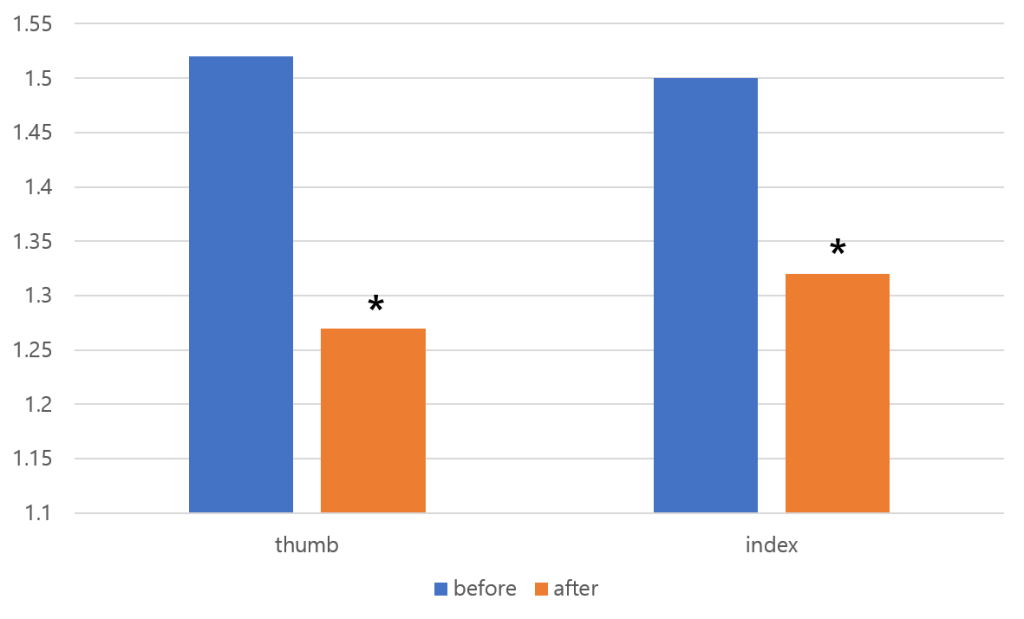
The mean MAS scores at pre-treatment were 1.50±0.36 for the wrist flexor, 1.52±0.34 for the thumb flexor, and 1.50±0.30 for the index finger flexor. After treatment, the mean MAS scores were significantly reduced to 1.25±0.26, 1.27±0.30, and 1.32±0.33, respectively. Statistical analysis confirmed that the reductions in MAS scores for the wrist flexor, thumb flexor, and index finger flexor were significant when compared to pre-treatment values (wrist flexor, p = 0.002, Z = -3.162; thumb flexor, p = 0.002, Z = -3.162; index finger flexor, p = 0.020, Z = -2.333)(Fig. 1).
User feasibility test
Overall, patient feedback was positive (see Table 1 for detailed data).
| Donning and doffing | |||||
| Easy to don and doff | Easy (18,90%) | Moderate (2,10%) | Difficult (0, 0%) | ||
| Duration (minutes) | <3 (15,75%) | 3~5 (4,20%) | >5 (1,5%) | ||
| Optimal positioning | Yes (18,90%) | Moderate (2,10%) | No (0,0%) | ||
| How many helpers? | 0 (18,90%) | 1 (2,10%) | 2 (0,0%) | ||
| Wrist extension | |||||
| Easy to operate? | Easy (20,10%) | Moderate (0,0%) | Difficult (0,0%) | ||
| Stretch to wanted angle? | Easy (19,95%) | Moderate (1,5%) | Difficult (0,0%) | ||
| Sustain the extended posture? | Easy (20,100%) | Moderate (0) | Difficult (0) | ||
| Finger extension | |||||
| Easy to operate? | Easy (20,100%) | Moderate (0,0%) | Difficult (0,0%) | ||
| Stretch to wanted angle? | Easy (20,100%) | Moderate (0,0%) | Difficult (0,0%) | ||
| Sustain the extended posture? | Easy (20,100%) | Moderate (0,0%) | Difficult (0,0%) | ||
| All the fingers extended equally? | Easy (10,50%) | Moderate (5,25%) | Difficult (5,25%) | ||
| General point | |||||
| Too heavy? | No (20,100%) | A bit (0,0%) | Heavy (0,0%) | ||
| Firm support? | Yes (20,100%) | A bit (0,0%) | No (0,0%) | ||
| Any trouble? | No (18,90%) | A bit (2,10%) | Yes (0,0%) | ||
| Willing to use? | Yes (20,100%) | A bit (0,0%) | No (0,0%) | ||
The numbers in parentheses indicate the tallies of patients who responded.
However, when assessing finger extension, only 10 patients (50%) reported that all fingers were easily extended, suggesting that the finger module required improvement to ensure equal extension of all fingers. Based on this feedback, we focused on enhancing the finger module by incorporating a ballooning ball mechanism in Figure 2.
This design features a flexible and resilient rubber ball, a metal upright pole, and an air pump connected to a manually operated cuff in Figure 3.
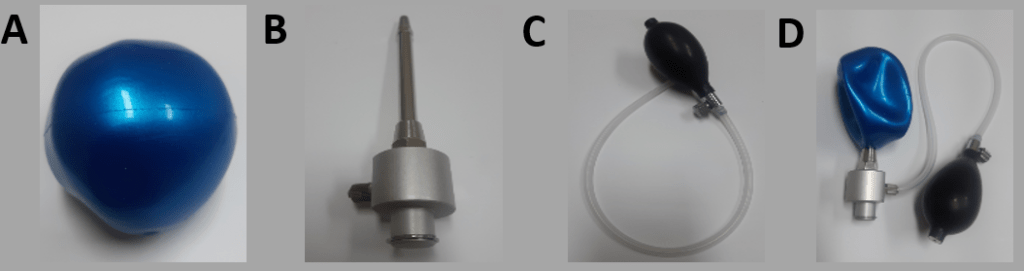
In its resting state, the ball remains deflated, allowing the metal upright pole to support the spastic hand as it fits into the finger module. When the cuff is used to inflate the ball, the expanding ball stretches the spastic hand and fingers in Figure 4.

We applied the upgraded device to all 20 patients and reassessed the user feasibility, specifically focusing on finger extension (see Table 2 for detailed data). Following the upgrade, all patients reported that all fingers were equally and easily extended. Additionally, all patients indicated that they could easily operate the device, achieve the desired angle of extension, and maintain the extended posture.
| Finger extension | |||
| Easy to operate? | Easy (20,100%) | Moderate (0,0%) | Difficult (0,0%) |
| Stretch to wanted angle? | Easy (20,100%) | Moderate (0,0%) | Difficult (0,0%) |
| Sustain the extended posture? | Easy (20,100%) | Moderate (0,0%) | Difficult (0,0%) |
| All the fingers extended equally? | Easy (20,100%) | Moderate (0,0%) | Difficult (0,0%) |
The numbers in parentheses indicate the tallies of patients who responded.
3. Discussion
In this study, we examined the effects of a simple stretching device for the wrist and hand, developed specifically to manage spasticity in chronic stroke patients. After using the device for 1 month, patients exhibited significant reductions in spasticity, as measured by the MAS, in the wrist flexor, thumb flexor, and index finger flexor muscles. Additionally, patient feedback revealed a key limitation of the initial device: not all fingers were easily extended. In response to this feedback, we modified the device by incorporating a ballooning ball mechanism, which effectively allowed for the equal extension of all fingers. All participants reported satisfaction with the modified device.
Previous efforts to develop stretching devices for managing hand spasticity have been made14. However, these devices were limited in their ability to control spasticity in the fingers without addressing wrist spasticity. Additionally, earlier devices often required assistance for donning and operation, limiting their practicality for independent use. In contrast, our device addresses spasticity in both the fingers and wrist and is designed for independent use by the patient. This independence allows patients to use the device as frequently as needed, facilitating more consistent management of spasticity. Feedback from our patient survey further highlighted the device’s ease of use, including its straightforward donning and doffing process, user-friendly module manipulation, and portability.
Another critical advantage of our device is its ability to maintain the forearm in a neutral position. Previous devices often positioned the forearm in a prone position, complicating the fitting process and causing discomfort in the spastic upper limb made14. When the wrist and fingers are flexed due to spasticity, a prone forearm position hinders proper accommodation of the flexed joints, potentially leading to additional strain on the wrist during stretching. Our device avoids these issues by supporting the forearm in a neutral position, making it easier and more comfortable to fit the spastic limb into the device. Moreover, the device applies stretching forces that are evenly aligned with the wrist and finger joints, preventing undue stress on the joints and ensuring a more effective treatment process.
Our study was conducted without a control group. However, we specifically recruited patients who were at least 12 months post-stroke. Given this timeframe, it is unlikely that the observed reductions in spasticity were due to natural recovery. Therefore, although we did not compare the therapeutic outcomes of our stretching device with a control group, our results suggest that the device is effective in managing spasticity in the wrists and hands of chronic stroke patients.
The user survey revealed that patients had some issues with the original finger module, particularly with uneven stretching of the fingers. The rigid plastic module was not well-suited to accommodate spastic fingers, especially at the interphalangeal joints. In response to this feedback, we redesigned the finger module, incorporating an inflatable ball with an upright bar and an air nozzle to serve as a guide pole. This design made it easier for spastic hands to fit into the module. We integrated a puffing device from a sphygmomanometer into the air infusion system, allowing the ballooning ball to provide a flexible and comfortable contour for the fingers, both at rest and during stretching. With the initial device, some severely spastic fingers could escape during stretching, exacerbating the spastic posture. The redesigned module, with its ballooning ball concept, applied fluid pressure evenly across the fingers, ensuring uniform stretching.
In conclusion, our stretching device effectively alleviated wrist and hand spasticity in chronic hemiparetic stroke patients, and its feasibility was confirmed through user feedback. Moreover, by incorporating the insights from the user survey, we upgraded the device, leading to enhanced patient satisfaction. However, our study has limitations. It was conducted without a control group, and we did not evaluate the therapeutic outcomes of the modified device. Additionally, we did not monitor serial changes in MAS scores during the 1-month treatment period, nor did we investigate the long-term effects of the treatment. Therefore, further studies are warranted to address these limitations.
4. Methods
We prospectively recruited 20 consecutive stroke patients (M:F = 9:11, age = 68.7±4.4, cerebral infarct:cerebral hemorrhage = 7:13, right hemiplegia:left hemiplegia = 11:9, time between onset and start of clinical trial = 13.4±1.1) based on the following inclusion criteria: 1) ≥12 months after stroke onset; 2) hemiparesis or hemiplegia due to stroke; 3) sufficient cognitive ability to understand the clinical trial process and respond to our questionnaire; 4) spasticity in the wrist flexor, thumb flexor, and index finger flexor with a modified Ashworth scale (MAS) score between 1 and 2; 5) no history of musculoskeletal disease (e.g., arthritis, musculotendinous injury, or bone fracture) or peripheral nerve injury in the affected upper extremity. The Ethics Committee of the Korea National Institute for Bioethics Policy approved this protocol, and all patients provided written informed consent before participating in the study.
Stretching device and intervention
The device comprises a forearm support module, a wrist module, and a finger module. Most components were fabricated from plastic using 3D printing techniques. The device lacks electronic controls or a motorized system, ensuring ease of use and safety for users. The primary function of the device is to stretch and extend the spastic wrist and fingers, allowing individuals to operate it independently without assistance. The forearm support module stabilizes the patient’s forearm during stretching (Fig. 1), providing a base upon which the wrist module can rotate to achieve dorsal wrist extension. A rotational axis between the hand and forearm modules allows for easy wrist stretching, and the wrist can be securely fixed at any point using a locking system. The finger module, designed ergonomically for spastic hands and fingers, comfortably and securely holds the patient’s fingers. It stretches the fingers by widening the gap between the thumb and the other fingers, controlled by rotating a wheel. The module can also be fixed at any desired position. Participants used the device independently, four times daily, 7 days a week, for 1 month. Each stretching session was maintained for a minimum of 15 minutes and a maximum of 20 minutes. All the participants received conventional rehabilitation during the intervention period. No medications or procedures influencing spasticity were changed during the study period.

Assessment of spasticity
The degree of spasticity was evaluated using the MAS for the wrist flexor, thumb flexor, and index finger flexor (Kim et al., 2013). MAS assessments were conducted immediately before the first therapeutic session with the device (pre-treatment) and again 1 day after the final session (post-treatment). The MAS scores were defined as follows: 1—slight increase in muscle tone, indicated by a catch and release or minimal resistance at the end of the range of motion (ROM) during flexion or extension; 1+—slight increase in muscle tone, indicated by a catch followed by minimal resistance throughout less than half of the ROM; 2—more marked increase in muscle tone through most of the ROM, although the affected part(s) could still be moved easily. For statistical analysis, scores of 1, 1+, and 2 were assigned values of 1, 1.5, and 2, respectively.
User feasibility assessment
A questionnaire was administered to the participants to identify the device’s potential shortcomings and assess its convenience. The questionnaire included the following items:
A. Donning and doffing
• Is it easy to don and doff?
• How long does it take to don and doff?
• Does the device provide optimal positioning for the wrist and fingers?
• How many helpers are required to don and doff?
B. Wrist extension
• Is the wrist module easy to operate?
• Can the wrist be stretched to the desired angle?
• Can the extended posture and angle be easily maintained?
C. Finger extension
• Is the finger module easy to operate?
• Can the fingers be stretched to the desired angle?
• Can the extended posture and angle be easily maintained?
• Are all the fingers equally extended and stretched?
D. General points
• Is the device too heavy to carry?
• Does the baseplate provide firm support?
• Are there any inconveniences during use?
• Would you be willing to use the device daily to manage hand spasticity?
Statistical analysis
Data were analyzed using SPSS Statistics for Windows, version 27.0 (IBM Corp., Armonk, NY, USA). To verify normal data distributions, Kolmogorov–Smirnov tests were performed prior to each analysis. As the data were not normally distributed, we compared pre-treatment and post-treatment MAS scores using the Wilcoxon signed-rank test. Statistical significance was set at p < 0.05.
References
- Ivanhoe, C.B., Reistetter, T.A. (2004). Spasticity: the misunderstood part of the upper motor neuron syndrome. Am J Phys Med Rehabil. 83(10 Suppl):S3-9. Raciti, L., Raciti, G., Ammendolia, A., de Sire, A., Onesta, M.P., Calabrò, R.S. (2024). Improving Spasticity by Using Botulin Toxin: An Overview Focusing on Combined Approaches. Brain Sci. 14(7):631 [↩]
- Gallichio, J.E. (2004).Pharmacologic management of spasticity following stroke. Phys Ther. 2004;84(10):973-81 [↩]
- Ryu, J.S., Lee, J.W., Lee, S.I., Chun, M.H.(2010). Factors predictive of spasticity and their effects on motor recovery and functional outcomes in stroke patients. Top Stroke Rehabil 17(5):380-8 [↩]
- Chang, M.C., Boudier-Revéret, M.(2020). Management of elbow flexor spasticity with ultrasound-guided alcohol neurolysis of the musculocutaneous nerve. Acta Neurol Belg. 20(4):983-984. [↩]
- Chang, M.C., Choi, G.S., Boudier-Revéret, M.(2021). Ultrasound-guided ethyl alcohol injection to the deep branch of the ulnar nerve to relieve hand spasticity in stroke patients: A case series. Transl Neurosci. 2(1):346-350. [↩]
- Chang, M.C., Choo, Y.J., Kwak, S.G., Nam, K., Kim, S.Y., Lee, H.J., Kwak, S.(2023). Effectiveness of Extracorporeal Shockwave Therapy on Controlling Spasticity in Cerebral Palsy Patients: A Meta-Analysis of Timing of Outcome Measurement. Children (Basel). 10(2):332. [↩]
- Hampton, C.(2024). The Use of Long-Arm Serial Casting to Manage Multiple Sclerosis Spasticity: A Case Report. Int J MS Care. 26:144-148. T Tilborg, N.A.W.V., de Groot, V,, Meskers, C.G.M.(2024) The effectiveness of early interventions for post-stroke spasticity: a systematic review. Disabil Rehabil. 1-12 [↩]
- Selles, R.W., Li, X., Lin, F., Chung, S.G., Roth, E.J., Zhang, L.Q.(2005). Feedback-controlled and programmed stretching of the ankle plantarflexors and dorsiflexors in stroke: effects of a 4-week intervention program. Arch Phys Med Rehabil. 86(12):2330-6( [↩]
- Wu, C.L., Huang, M.H., Lee, C.L., Liu, C.W., Lin, L.J., Chen, C.H.(2006). Effect on spasticity after performance of dynamic-repeated-passive ankle joint motion exercise in chronic stroke patients. Kaohsiung J Med Sci. 22(12):610-7 [↩]
- Zhang, L.Q., Chung, S.G., Bai, Z., Xu, D., van Rey, E.M., Rogers, M.W., Johnson, M.E., Roth, E.J.(2002) Intelligent stretching of ankle joints with contracture/spasticity. IEEE Trans Neural Syst Rehabil Eng. 10(3):149-57 [↩]
- Chang, P.H., Lee, S.H., Gu, G.M., Lee, S.H., Jin, S.H., Yeo, S.S., Seo, J.P., Jang, S.H.(2014) The cortical activation pattern by a rehabilitation robotic hand: a functional NIRS study. Front Hum Neurosci. 8:49. [↩]
- Jo, H.M., Song, J.C., Jang, S.H.(2013). Improvements in spasticity and motor function using a static stretching device for people with chronic hemiparesis following stroke. NeuroRehabilitation. 32(2):369-75. [↩]
- Kim, E,H,, Chang, M.C., Seo, J.P., Jang, S.H., Song, J.C., Jo, H.M.(2013) The effect of a hand-stretching device during the management of spasticity in chronic hemiparetic stroke patients. Ann Rehabil Med. 37(2):235-40 [↩]
- Chang, P.H., Lee, S.H., Gu, G.M., Lee, S.H., Jin, S.H., Yeo, S.S., Seo, J.P., Jang, S.H.(2014) The cortical activation pattern by a rehabilitation robotic hand: a functional NIRS study. Front Hum Neurosci. 8:49. Jung, Y.J., Hong, J.H., Kwon, H.G., Song, J.C., Kim, C., Park, S., Kim, Y.K., Ahn, S.H., Jang, S.H.(2011). The effect of a stretching device on hand spasticity in chronic hemiparetic stroke patients. NeuroRehabilitation. 29(1):53-9 [↩] [↩]