Abstract
This literature review will discuss the research focused on stroke, post-traumatic stress disorder (PTSD), and post-stroke PTSD. A stroke is when the blood supply to a part of the brain gets rapidly reduced or completely cut off. The two types of strokes are ischemic and hemorrhagic strokes. There are also several signs of a stroke: numbness, weakness, paralysis, and more. Stroke is a serious medical emergency that has an extensive list of side effects, such as motor, cognitive, and/or emotional impacts. One often overlooked complication of stroke includes one’s development of post-traumatic stress disorder (PTSD). PTSD is a stress- and trauma-related disorder that develops in some people who have encountered extreme amounts of trauma. The typical symptoms of PTSD are anxiety, depression, being in fight or flight mode, and so much more. Research has shown that there is a positive bidirectional relationship between a stroke and PTSD. However, technology is not advanced enough to detect PTSD, and even post-stroke PTSD, in its early stages, making them both harder to treat. The suggested treatments range from using medications to aggressive therapies in order to treat post-stroke, and regular, PTSD. The overall assessment shows that post-stroke PTSD is more common than people think and that there needs to be more research, advancement in technology, and advancement in therapies in order to combat it. Here, I will explore the overall relationship between stroke and PTSD and highlight work being done to assist in patient recognition and recovery.
Introduction
Every 40 seconds, someone has a stroke, and every 4 minutes, someone dies from a stroke1. A stroke is a severe medical complication that results in damage to the brain. The normal human brain will look different than the brain of a person who has suffered a stroke. A healthy human brain has blood flowing in and out, distributing nutrients that are essential for the brain and body to function. The human brain has neurons, glial cells, astrocytes, and many other components that assist in healthy brain function2. However, when someone suffers a stroke, an area of the brain is damaged and the brain’s default functions are disrupted. The area of stroke damage relates to the stroke symptoms an individual might develop. A stroke occurs when the blood supply to a part of the brain gets severely reduced or blocked. There are two types of stroke: ischemic and hemorrhagic. An ischemic stroke is when the blood supply to the brain gets blocked or cut off. A hemorrhagic stroke is when a blood vessel in the brain leaks or bursts. Based on the area of the brain that is damaged by a stroke, one can have different symptoms. The motor side effects for post-stroke patients can range from not being able to write to being severely paralyzed. In addition to the physical and behavioral effects of a stroke, there is also a serious impact on one’s mental health. One of the severe complications of a stroke is post-traumatic stress disorder (PTSD). Studies show that roughly 25% of stroke patients will develop PTSD as a result of their stroke. This paper will discuss stroke, PTSD, and the relationship between the two3.
Stroke
A stroke is when the blood supply to a part of the brain gets severely reduced or blocked, of which there are two types: ischemic and hemorrhagic4. An ischemic stroke is when the blood supply to a part of the brain gets reduced or blocked. As a result, this prevents the tissues in the brain from getting oxygen and other nutrients that are necessary for the tissues to function. So, the brain cells in these tissues get damaged immediately and start to die. The other type of stroke is hemorrhagic5. This is when a blood vessel in the brain bursts or leaks. This causes a bleed in the brain. The blood puts a lot of pressure on the brain cells. And, as a result, the brain cells begin to rapidly die. There are a couple of causes of strokes. The cause of an ischemic stroke is when an artery is clogged or blocked in the brain. Blocked arteries and/or blood vessels can be caused by the build-up of fatty deposits, blood clots, and/or other debris. Most of the debris that causes blocked blood vessels comes from the heart5. The cause of a hemorrhagic stroke is when a blood vessel leaks or bursts in the brain. There are many causes of a ruptured blood vessel. One is high blood pressure that is not under control. Bulges at weak spots in the blood vessels are called an aneurysm. Any head trauma, such as a car accident, makes blood vessels susceptible to rupture. And, an ischemic stroke can even lead to a hemorrhagic stroke. Between the two types of strokes, an ischemic stroke is more common than a hemorrhagic stroke5.
Influences, Symptoms, and Complications of Stroke
There are many physical influences of stroke. However, there can be cultural, socioeconomic, and demographic causes behind a person suffering from a stroke. Physical aspects such as age, health, and mental capability play crucial roles in whether a person is at risk of having a stroke. Nonetheless, different demographics such as ethnicity, religion, income, sex, education, location, etc., can also make a person more prone to stroke.
Firstly, one study sought to see whether socioeconomic status could be a factor in influencing stroke6. This was a relatively large study, consisting of 86,316 patients, all of whom were diagnosed with an ischemic stroke and were from a wide variety of different demographics. Patients’ education level (primary, secondary, undergraduate, and postgraduate) was used as the metric for socioeconomic status. This study used the Reaction Level Scale to measure the severity of stroke in all the patients. The results showed that patients with a low socioeconomic status were associated with a high risk of severe stroke. In contrast, the patients with a medium to high socioeconomic status were not at as high a risk of stroke as the low socioeconomic status patients were. This study revealed that about one-third of the reason for the strong association between low socioeconomic status and high risk for severe stroke was due to people with low socioeconomic status having unique risk factors. These unique risk factors led to a high risk for severe stroke7. Nevertheless, demographic influencers can also play a part in how patients are treated in post-stroke care. For example, one study focused on how socioeconomic status could affect patients with stroke and the post-stroke care that patients from different socioeconomic statuses received. Most of the evidence on how socioeconomic status affects stroke, and post-stroke care, demonstrates that people who have low socioeconomic status are more prone to having high levels of hypertension (high blood pressure), hyperlipidemia (high levels of lipids in the blood, which can lead to a high risk for stroke), drinking problems, smoking, obesity, and a sedentary lifestyle (a lifestyle without adequate exercise). This study also found that people with low socioeconomic status are less likely to receive proper post-stroke care. This means they can experience inadequate rehab, unfit treatments, poor management of risk factors post-stroke, and restrictive access to high-quality post-stroke care. All of these subpar experiences in post-stroke care create inequality in the healthcare industry, making it harder for people of low socioeconomic status to get the treatment they deserve in their post-stroke care plan. Overall, people of low socioeconomic status are less likely to get proper treatment post-stroke. As a result, low socioeconomic people can be in danger of a wide variety of complications, such as post-stroke PTSD, that could emerge post-stroke due to their insufficient post-stroke care8. Through these studies, it is apparent that post-stroke patients of low socioeconomic class are most likely to receive insufficient care; therefore, they can face a wider variety of complications post-stroke and have a higher potential to suffer more. Undeniably, a stroke can cause serious brain injury; therefore, there are some symptoms and complications that doctors look out for. Some of the most obvious signs of a stroke are numbness, weakness, and/or paralysis in the body. For example, if someone’s smile is lopsided or if their arms are falling down, this person is potentially having a stroke. Another symptom of a stroke is when someone cannot speak properly, evidenced by slurring or an inability to understand a simple sentence another person is saying. Other symptoms include difficulty walking, vision problems, and a severe headache. Since a stroke is a severe brain injury, it will have some harmful complications. After an individual has a stroke, they may become paralyzed. They may have trouble talking, swallowing, and eating. Further, they may have trouble with speaking, understanding speech, writing, and/or reading, which is dependent on the area of the brain that is damaged from the stroke. Other obvious complications of strokes include memory loss, trouble thinking, and trouble forming clear thoughts. Two other severe complications of a stroke are Dementia and Alzheimer’s Disease. All of these complications are indicators of how severe a person’s stroke was. However, the NIH Stroke Scale, a type of Reaction Level Scale, is used to determine how serious one’s stroke was. The NIH Stroke Scale asks an individual to perform physical and mental tasks in order to evaluate how severe their stroke was. The NIH Stroke Scale can also help medical professionals determine a patient’s neurological function and stroke severity9.The two complications of strokes that overlap the most with mental health are emotional symptoms and changes in behavior. After a stroke, a person may have trouble controlling their emotions. An individual could also become more withdrawn and might develop depression after suffering a stroke. The behavioral and emotional symptoms that can develop after a stroke can be the cause of post-traumatic stress disorder (PTSD) that a person might have. Studies have shown that women are more subject to strokes than men with one in four women having a chance of stroke after the age of twenty-five5.
| Stroke complications | PTSD connections |
| Anxiety | ↑, ↔ |
| Seizures | ↓ |
| Paralysis | ↓ |
| Dementia | ↑, ↤ |
| Depression | ↑, ↔ |
| Memory loss | ↑, ↔ |
| Alzheimer’s Disease (AD) | ↑, ↦ |
| Poor emotional regulation | ↑, ↔ |
| Trouble with talking and eating | ↓ |
| Trouble thinking and forming clear thoughts | ↑, ↔ |
One complication of stroke is post-stroke PTSD, which is a topic that has been researched and is probable to continue to be a topic of research for a long time to come. Usually, there are signs of post-stroke PTSD and PTSD in general. Common side effects of post-stroke PTSD are post-stroke depression (PSD), anxiety, and fatigue10. These three complications need to be diagnosed early on in post-stroke patients to prevent any of these symptoms from worsening. Two of the most detrimental diseases a person can get after having a stroke are Dementia and Alzheimer’s Disease (AD). This study has also outlined that there is a 20% chance for the development of early-onset dementia to develop in post-stroke patients within the first 6 months after a stroke. 50% of post-stroke patients were diagnosed with epilepsy who are over the age of 60-years-old. Other complications can be falls and any other injuries, all of which can land post-stroke patients back in the hospital for further treatments. Almost 50% of post-stroke patients develop chronic pain, but chronic pain is often not caught in time for there to be any prevention of it. There are countless other complications for post-stroke patients that cannot be identified early on in their recovery, making it more likely these post-stroke patients will develop one or more of these awful complications11. Another serious complication of a stroke is seizures. Recent studies have shown that post-stroke seizures have become more and more prevalent in post-stroke patients. Post-stroke seizures can be caused by long-term hospitalization and can lead to an increased mortality rate. However, long-term hospitalization is often necessary as some post-stroke patients have to stay in the hospital for treatments and screenings. So, although long-term hospitalization is useful, it can often lead to unintended negative side effects, such as a dwindling social support system. The standard way to treat seizures is through anti-epileptic drugs (AEDs), however, research is lacking on the side effects of these drugs for post-stroke patients. However, there are no proven studies or theories that allow post-stroke patients specifically to take AEDs for their post-stroke seizures, due to a lack of research support in this area. In order to determine the best treatment for post-stroke seizures, there needs to be more studies on this specific subject. Since seizures are one of the most detrimental complications in post-stroke patients, putting this topic at the forefront of post-stroke research is a must in order to prevent post-stroke seizures12.
Therapeutics and Medications for Stroke
As stroke impacts more than 795,000 people in the United States yearly, many resources and research dollars have been funneled to develop therapeutics and medications used to treat post-stroke patients13. Endovascular therapy is a procedure used to treat ischemic stroke, wherein a doctor places a catheter into the brain that removes the clot that is causing the stroke. Endovascular therapy has high success rates. However, it is very invasive, which means there are a host of complications that go along with the procedure. Studies have shown that the top three complications of endovascular therapy are pneumonia, cardiac insufficiency, and myocardial infarction. However, if doctors can identify any of these complications in their early stages, it is possible to prevent or lessen their brunt14. Another type of therapy used for post-stroke patients is underwater exercise training. Underwater exercise training is when post-stroke patients exercise underwater and receive the routine treatment plan for a stroke. Studies show that underwater exercise training improves walking ability, balance, and overall mobility in post-stroke patients which can lead to fewer physical complications of a stroke15. This type of training is crucial in order for a post-stroke patient’s mobility because of the complications someone can experience after suffering a stroke. Paralysis, trouble walking, and trouble moving limbs are all common complications in post-stroke patients. Using underwater exercise training can decrease, or completely avoid, the effect of any of these complications. Other, more serious, complications in post-stroke patients are seizures and epilepsy. There have been some studies done to show that the drug diazepam can reduce or prevent the seizure rate in post-stroke patients. In one study, patients who were given diazepam for three days did not have any seizures in the first three months after a stroke. So, diazepam is verified to work for that time period, but there is a lack of research focused on how diazepam can affect someone after long-term usage. However, there need to be more studies done on the prevention and overall treatments for post-stroke seizures16.
Another treatment used for post-stroke complications related to mobility is constraint-induced movement therapy (CIMT). CIMT is the most studied treatment for mobility problems related to post-stroke PTSD, therefore it is the most reliable treatment overall for post-stroke patients. CIMT is mainly used for upper limb impairments. The therapy consists of the patient’s non-affected limb being tied up to force the patient to use the affected limb to complete tasks such as picking up an object or flipping a switch. The repetition and consistency of this therapy can significantly regenerate the ability of the affected limb. The results of CIMT show that it improves and benefits motor function, arm/hand activities, and overall function in daily life. However, the mechanisms of CIMT are still poorly understood by doctors and physicians. As such more studies and clinical trials are needed to thoroughly understand how CIMT helps patients17. Another complication of a stroke is post-stroke cognitive impairment (PSCI). PSCI is treated with many medical screenings and routine post-stroke therapy. However, PSCI can lead to two more detrimental complications of a stroke: Dementia and Alzheimer’s Disease, both of which take a heavy toll on a person’s quality of life18. Lastly, there is the common complication of post-stroke post-traumatic stress disorder (PTSD), which researchers have aimed to investigate. One way to treat post-stroke PTSD is through preventative therapy. The crux of this treatment is to use different ways to prevent post-stroke PTSD. In contrast, supportive therapy is also used to treat post-stroke PTSD. Supportive therapy is a way to support or aid someone who has post-stroke PTSD rather than prevent it19.
PTSD
One in four stroke patients suffers from post-traumatic stress disorder (PTSD). Although many people endure trauma at some point in their lives, the development of PTSD is quite rare, which explains why there is a gap in research in regard to PTSD20. PTSD is a stress-related disorder that develops in some people who have experienced excessive amounts of trauma. As such, it is clear that PTSD is a severe disorder that can affect the mental health of the person dealing with it.
Symptoms and Ranking of PTSD
As previously mentioned, PTSD is a stress-related disorder that develops in some individuals who have experienced a lot of trauma. Early on, PTSD was dubbed as an anxiety-related disorder21. But, after many studies were conducted, it was shown that PTSD is a trauma- and stress-related disorder. Some common symptoms of PTSD are anxiety and depression. Other symptoms that are unique to PTSD are intrusive experiences, avoidance, mood swings/changes, and arousal. Studies show that people with PTSD, and anxiety, have a hard time separating safety from danger and are still fearful or on fight or flight mode in safe situations21. Fight or flight mode is a stress response. The fight or flight response is when many hormones are released and tell the body to either stay and fight or to run and get out of harm’s way. During fight or flight, the body’s number one priority is to keep itself safe from any precarious situations22. There have been studies done on the behaviors of people with PTSD and the consequences of them. Studies on war veterans show that people with PTSD have different and difficult behaviors but they do not show any signs of increased levels of aggression to the point where they could physically hurt people23. Other emotions associated with PTSD are the following: negativity, neuroticism (impaired emotional stability), harm avoidance, novelty-seeking (impulsivity and loss of temper), hostility, anger, and anxiety20.
Other symptoms of PTSD that have been studied are avoidance and numbing. Studies have shown though that both of these symptoms are associated with PTSD, but they are particularly hard to treat as many treatments could help one and worsen the other symptom. The data gathered in randomized trials suggests that (a) different treatments have effects on reducing avoidance but not numbing, (b) patients with more severe numbing have worse treatment outcomes than patients who have the symptom of avoidance, (c) avoidance and numbing have different patterns with depression which are why they are hard to treat at the same time, and (d) avoidance and numbing also have different correlations with physiological aspects. However, there have not been comprehensive studies conducted on the various symptoms of PTSD, hence why there are only a selective number of treatments that yield positive results. There needs to be more studies done on the numerous symptoms of PTSD in order to develop more advanced treatments to treat the variety of PTSD symptoms24. Furthermore, if a person is suspected of suffering from PTSD, they would go through a test to be clinically diagnosed with PTSD. There is a ranking scale, the Clinician-Administered PTSD Scale (CAPS), used to determine if a person has PTSD. If a person has PTSD, then this ranking scale can determine the severity of the PTSD as well. A unique feature of CAPS is the ability to provide specific questions that correspond with the specific types of PTSD that were diagnosed. CAPS is the most used test to diagnose PTSD and consists of 30 questions that take about 45-60 minutes to fill out. 20 of these questions ask about PTSD symptoms, while the other 10 questions ask about the response, severity, frequency, etc. of these symptoms. Those 10 questions are answered on a scale from 0-5, 0 being the question is irrelevant for the person taking the CAPS, and 5 being the question greatly affects the person taking the CAPS. The CAPS can be used to make a current diagnosis of PTSD, a lifetime diagnosis of PTSD, and assess the symptoms of PTSD25.
Subtypes of PTSD
Research shows that there are three subtypes of PTSD: internalizing, externalizing, and low pathology. Internalizing PTSD is usually keeping to oneself, being depressed, and having high levels of anxiety. Studies showed that internalizers dealt with severe depression, hypochondriasis (an obsession with the idea of having a serious yet undiagnosed medical condition), and low positive affections. Externalizing PTSD is the exact opposite. This is when someone with PTSD lashes out, physically hurts people, and has aggression problems. Studies showed that externalizers were found to have high levels of aggression, hostility, and even harmful substance abuse. Low pathology PTSD is when a person with PTSD has stable emotions and can function relatively normally despite being diagnosed with PTSD. Out of the three subtypes of PTSD, low pathology PTSD is definitely the subtype that is the most controlled. Internalizing and externalizing PTSD people are at a higher risk for mortality than people with low pathology PTSD because internalizers and externalizers present more severe psychiatric and behavioral aggravations. Therefore, it is reasonable that internalizers and externalizers deviate in more extreme directions and result in further distress26.
Another subtype of PTSD is Dissociative PTSD (D-PTSD). D-PTSD is associated with depersonalization (when an individual senses that circumstances are not real) and derealization (feeling detached from one’s surroundings). The complex and damaging component of D-PTSD is that it can interfere with the treatment course and outcome. Few studies have been conducted that have shown there are subtypes of D-PTSD, but the research is conflicting. Some studies say there are only three subtypes of PTSD (internalizing, externalizing, and low pathology; Flood et. al, 2010), whereas other studies claim there are subtypes of D-PTSD. However, the studies that have been done on D-PTSD have shown that clear-cut signs of D-PTSD are over-activation of frontal cortical activity which can lead to the overexcitement of the limbic system (the hippocampus and amygdala). These signs in D-PTSD support the evidence gathered for regular PTSD which shows hyper, and unrestrained, activity in the limbic system. There have also been studies done on the genetic component, or variable, that could be at play and cause D-PTSD. For example, one study showed that twins have a 50% chance of getting D-PTSD, and twins have an even higher chance than 50% of getting D-PTSD if they are in an adoption program27.
Genetic Factors in PTSD
Studies show that both PTSD and lifetime trauma exposure (LTE) can be genetically inherited. Several alleles and genes can cause a person to be more likely to get PTSD, or even LTE, in their life. Research has also focused on neuroanatomical changes (i.e. changes in brain structure or connectivity) in response to having PTSD. Studies have shown that people who have PTSD have an abnormal morphology of their hippocampus. The hippocampus is involved in short-term memory regulation, learning, and emotion. People with PTSD are known to have trouble controlling their emotions. The cause of irregular emotions in people with PTSD could be an abnormal morphology such as in one’s hippocampus. However, many studies have reported that there needs to be more research surrounding the relationship between neuroanatomy and PTSD in order to determine preventatives and treatments for abnormal hippocampal morphology. In the future, studying individuals who are at high risk for trauma (i.e. soldiers, veterans, firefighters, etc) could yield more conclusive results in this field. The research could involve these high-risk individuals getting brain scans, to observe the different brain regions, before and after they endure traumatic events. This can show whether there is an abnormal neural morphology in individuals with PTSD. It also would not be surprising to find that other regions of the brain, in addition to or instead of the hippocampus, are altered due to PTSD28. Other studies have also been conducted on the genetic components related to PTSD. Studies show that people who have PTSD also have abnormal qualities in the hypothalamus region. Some studies have shown that there is a relationship between Neuropeptide Y (NPY) and PTSD. NPY is primarily a fear reductive, meaning it calms the mind down. So, since people with PTSD usually have a hard time controlling their emotions, there could be low levels of NPY in the hypothalamus region29.
Cultural Influence on PTSD
There are many contributing factors when a person develops PTSD. The most obvious one is the environment around them. However, different demographics and cultural aspects can also play a role in influencing different people’s chances of developing PTSD. One study examined how prevalent PTSD was across different types of trauma exposures and different cultures. This study searched for papers that fit their criteria of research and found that refugees who were displaced into cultures that were similar to their own were at a higher risk of developing PTSD30. Similarly, another study synthesized evidence of how prevalent PTSD was in the United States. This study used data from 38 articles. The results showed that PTSD prevalence in civilians ranged from 8-56.7%, 2.3-9% in 1-year prevalence, and a lifetime prevalence of 3.4-26.9%. PTSD prevalence in people from the military ranged from 1.2-87.5%, 6.7-50.2% in 1-year PTSD prevalence, and a lifetime prevalence of 7.7-17%. According to the study, PTSD prevalence was more common in emergency responders, refugees, American Indians, Alaska Natives, individuals with heavy substance use, individuals with a past suicide attempt, trans-masculine individuals, and women with past military sexual trauma. Being female, having a lower income, being younger in age, and having behavioral health conditions were all identified as risk factors for PTSD31. Through some studies, evidence has been revealed that some subpopulations are at a higher risk of developing PTSD. However, there should be more research done on this specific topic to help the PTSD-vulnerable subpopulations in the future.
Therapeutics for PTSD
The therapies used to treat PTSD are different and more aggressive than therapies used to treat anxiety or anxiety-related disorders. The most popular, and most-studied, therapy for PTSD is psychotherapy21. Psychotherapy is when individuals with PTSD are forced to learn not to be fearful of everyone or every situation. The main goal of using psychotherapy is to reduce the patient’s reactivity to circumstances that trigger their PTSD episodes (i.e. fear extinction). This introduction to fear extinction in the patient is very helpful since fear is one of the most present symptoms of PTSD. There have also been sleep therapies or treatments used to help sleep disruption in PTSD patients. Treating sleep apnea (through continuous positive airway pressure [CPAP]), insomnia (usually through psychotherapy), and nightmares improves the symptoms of PTSD patients. In contrast, cognitive-behavioral therapies are used for anxiety-related disorders. There is also a pharmaceutical therapeutic approach of using selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors (SNRIs) to treat PTSD as well as anxiety-related disorders21. There is another type of therapy, exposure therapy, that is used to treat PTSD symptoms. Again, this is another aggressive, yet reliable, approach to treating and hopefully getting rid of PTSD. Exposure therapy is when the patients have to confront uncomfortable, yet realistic, stimuli that replicate what caused their PTSD until their PTSD symptoms are reduced or gone. There have been many studies done on exposure therapy and the results have shown that PTSD symptoms have decreased as a result of this therapy32. Studies show that exposure therapy is a safe option for treating PTSD as long as it is being administered by experienced therapists32. Nevertheless, since developing PTSD is rare, as mentioned earlier, there is limited research in this area. For example, research is lacking on how emotions relate PTSD to dementia and other diseases ( Table 1)23. Further, it is unknown how personality traits relate to or may manifest into PTSD20. As such, it is clear that more work is needed to uncover the possible causes, preventatives, and treatments for PTSD.
Stroke and PTSD
PTSD is an illness that can arise due to many neurological disorders, including a stroke. There have been many studies done on the bidirectional relationship between PTSD and stroke33. The two questions asked to further understand this relationship are: “Can having a stroke make a person more likely to develop PTSD?” and “Does having PTSD make it more likely for a person to have a stroke?”. Research has been conducted to explore these questions.
Many studies have been conducted to answer the first question: “Can having a stroke make a person more likely to develop PTSD?”. One study shows that 3% – 31% of post-stroke patients develop PTSD with a median of 16.5%33. Studies across the world have demonstrated that 1 in 4 post-stroke patients will develop PTSD, regardless of the severity of the stroke. That means 25% of post-stroke patients will develop PTSD, which is a large percentage of post-stroke patients. This explains why there has been a lot of research conducted on PTSD that can develop after a person suffers from a stroke. Post-stroke PTSD is typically associated with premorbid neuroticism (the existence of poor emotional stability before the occurrence of a physical or emotional disease; Tang et. al, 2022). If post-stroke patients develop anxiety or depression after their stroke, then it is very likely they will also develop PTSD as a result of their anxiety and depression (Table 1). Evidently, PTSD is associated with a host of symptoms such as trouble controlling emotions, withdrawal, hostility, anger, anxiety, etc., that can decrease the quality of life a person might have. In the present day, the treatments available for post-stroke PTSD are randomized treatment trials, counseling, and therapy, which have varied success rates. This is all the more reason why there should be more research on the relationship between PTSD and strokes so that there can be new discoveries in preventatives, cautionary screenings, treatments, and so much more33.
Post-stroke PTSD
Further research explored the prevalence of post-stroke PTSD in post-stroke patients. This study was specifically done with patients who had a stroke within a 5-year period. Researchers examined if the following factors had any effect on post-stroke patients developing post-stroke PTSD: different demographics (different ages, genders, etc), stroke history, disability, medical comorbidities (several medical diseases at the same time), depression, emotional support, physical health, and mental health. These researchers found that 18% of the post-stroke patients developed PTSD after their stroke. Being young in age, having recurring strokes, greater disability, and comorbidities increased these patients’ chances of developing post-stroke PTSD. However, being old in age, being married/having a partnership, and having emotional support decreased these patients’ chances of developing post-stroke PTSD. The patients who did develop post-stroke PTSD, not surprisingly, also developed poor mental and physical health, and their quality of life decreased substantially34.
Since PTSD is a trauma and stress-related disorder, it is no surprise that there have been studies on whether stress relates to post-stroke PTSD. This specific study focused on whether Acute Stress Disorder (ASD) can cause post-stroke PTSD. ASD is a mental health problem where a person can have excessive amounts of stress after enduring a traumatic event. However, if the stress symptoms of ASD last for more than a month, then it is clinically diagnosed as PTSD. The study organized two visits for their patients: the first one was 1-2 weeks after their stroke, and the second one was 6-12 weeks after their stroke. As such, the latest visit in this trial was about 3 months post-stroke. At both of these visits, the patients had to describe their symptoms, and, of course, there were tests at both of these visits measuring whether these patients had ASD, post-stroke PTSD, or both. The results of this study showed that 22% of the patients met the criteria for ASD in the first visit post-stroke. It also showed that 62.5% of the patients who showed signs of ASD on the first visit developed PTSD in the second visit. However, 28.6% of the patients who showed symptoms of PTSD in the second visit did not have any symptoms of ASD in the first visit. The results of this study show that without proper treatment for ASD symptoms, post-stroke PTSD can develop. This study shows that it is very important to diagnose ASD and post-stroke PTSD symptoms quickly so that there can be action taken on them (treatments, therapies, etc)35.
Early Intervention for Post-stroke PTSD
Since post-stroke PTSD is a devastating complication of a stroke, some propositions can be used as early interventions to either stop the manifestation of PTSD or severely reduce the symptoms of post-stroke PTSD. One study aimed to see whether early intervention, using supportive psychological therapy, would prevent PTSD from progressing in post-stroke patients. This study consisted of 170 stroke patients, all of whom had some symptoms of post-stroke PTSD. The patients in this study only had 1 stroke. These patients were split into 2 groups: psycho-therapy group 1 (received supportive psychological therapy) and control group 1 (did not receive supportive psychological therapy). After a 2-month follow-up, any patients who were diagnosed with post-stroke PTSD were then separated further into 2 more groups: psycho-therapy group 2 (received supportive psychological therapy) and control group 2 (did not receive supportive psychological therapy). After another 2-month follow-up, the researchers believed that the early intervention, using supportive psychological therapy, was not better than the standard care used to treat post-stroke PTSD. However, 6 months after this study started, the study showed that the early intervention, using supportive psychological therapy, was effective in treating post-stroke PTSD19. The conclusion that can be drawn from this study is that if early intervention is used to treat post-stroke PTSD or developing symptoms of post-stroke PTSD, then the results will take time to be seen. This means the results will most likely not be seen until around the 6-month mark or even further down the line of the recovery process. However, the main focus is that supportive psychological therapy, when used as a tool for early intervention, can be successful in treating post-stroke PTSD in its early stages. Since post-stroke PTSD is a complex disorder, it is difficult to catch it in its early stages without mistaking it for another disorder. Therefore, there have not been many early intervention treatments used and/or tested to treat post-stroke PTSD.
Comparing PTSD from Other Causes to Post-stroke PTSD
PTSD can come from a stroke and many other causes. One common way people develop PTSD is through traumatic experiences from war. Firstly, one study focused on the topic of whether psychological inflexibility (PIF) is a factor in PTSD and whether PIF could create a unique variance in PTSD. All of the 236 people used in this study were war veterans from Iraq and Afghanistan. The findings in this study showed that PIF created a unique variance of PTSD. PIF is when a person has a rigid response to unpleasant thoughts and feelings that interfere with their peace of mind or well-being. Some predictors of PIF are serving in the army, rank in the army, trauma severity, perceived threats, peritraumatic dissociation (a complex combination of trauma responses that include depersonalization, derealization, and emotional numbness), recent life stress, and degree of social support around oneself. These predictors of PIF had a medium effect in creating the unique variance of PTSD in war veterans of this study. Other factors of PIF include personality disorders such as neuroticism (negative emotions, poor self-regulation, trouble dealing with stress, overreaction to perceived threats, and tendencies to complain), extroversion (outgoing and high energy), openness to new experiences, agreeableness, and conscientiousness. These factors had a small effect on the unique variance created in PTSD of these war veterans. The results of this study demonstrate that there is a strong association between PIF and PTSD symptom severity in war veterans from this study36. This study shows that PIF has the potential to create a variance of PTSD in combat veterans, something that has not been seen in people with post-stroke PTSD specifically.
Another study aimed to see whether mild traumatic brain injury (mTBI) and PTSD would cause abnormal neuropsychological results in Operation Iraqi Freedom (OIF) and Operation Enduring Freedom (OEF) veterans. In this study, these veterans were placed into 3 groups: healthy controls (veterans who did not have mTBI or PTSD, n = 43), PTSD only (n = 48), and comorbid blast-induced mTBI and PTSD (n = 47). Specifically, the veterans in the third group most likely developed their mTBI from head trauma through bombs and explosions wherever they were deployed. Three factors were apparent in the veterans in this study: perceived cognitive complications (PCC), perceived emotional distress (PED), and processing speed (PS). The analyses revealed that there was a significant difference in the PS category between the comorbid group and the other two groups. The comorbid group also has the highest levels of PCC and PED, likely because the veterans in the comorbid group underwent the most head trauma and traumatic experiences in general. The results showed that the OIF/OEF veterans who had both mTBI and PTSD had higher levels of emotional distress and cognitive complications, both of which can negatively impact their lives. Another important finding was that the huge discrepancy in PS between the comorbid group and the other two groups was due to the high levels of PTSD in the comorbid group, not due to the mTBI37. This study shows that traumatic brain injury increases a person’s chances of not only having PTSD but also poses a greater variety of effects that can harm a person’s life immensely. Another important fact to note is that both combat-related PTSD and post-stroke PTSD involve traumatic brain injury to an extent, which is one similarity between the two.
Through many studies, it is clear that post-stroke PTSD and PTSD from other causes have their similarities and differences. For instance, the comparison of emotional regulation between the two types of PTSD reveals that both types of PTSD include poor emotional regulation (Table 1). One difference between the two types of PTSD is how the severity of trauma affects the severity of PTSD symptoms. With post-stroke PTSD, the trauma comes from the stroke, which is induced by the function of the blood vessels in the brain going awry. In contrast, the trauma with PTSD in combat veterans comes from the distress on the battlefield during wartime. Since the degrees of trauma are different for these types of PTSD, the severity of PTSD will be different as well. In post-stroke PTSD, the trauma comes in one wave, only when the stroke occurs, and the stroke is usually stopped in a small time frame. This leaves less time for there to be more trauma induced upon a person. However, war does not have a set time frame for when it will end, as compared to stroke. This leaves an indefinite time frame where there is an enormous amount of time during which war veterans can develop PTSD due to explosions, bombings, combat, etc. Due to the longer period of time for trauma to be induced in war veterans, the severity of PTSD from stroke, potentially, could be less severe than PTSD from combat. Overall, PTSD in combat veterans and post-stroke PTSD have some similarities as well as some key differences.
Ischemic Stroke, Transient Ischemic Attack, and PTSD
There have been studies done on the bidirectional relationship between ischemic strokes and PTSD. This study examined what percentage of post-ischemic stroke patients developed PTSD and what factors triggered this PTSD. Some of the hypothesized factors were lesion location (where the stroke happened in the brain), degree of disability (how disabled someone was after their stroke), age, gender, and marital status. The patients in this study had a stroke in the right cerebral hemisphere, left cerebral hemisphere, brainstem, or cerebellum. The results of this study showed that 12.9% of the post-stroke patients developed PTSD. Patients with a higher level of disability were more likely to develop post-stroke PTSD. The study also showed that the lesion location played a part in developing post-stroke PTSD. Patients who had a stroke in the right cerebral hemisphere and brainstem were more likely to develop post-stroke PTSD. This study found that post-stroke PTSD had no relation to age, gender, or marital status. More research is needed on the factors of post-stroke PTSD in order to diagnose it quickly and hopefully treat it so that it cannot progress or worsen38. Another study was conducted to observe the relationship between anxiety, depression, and PTSD. This study, just like the previous one, involved patients who specifically had an ischemic stroke. None of the patients had psychiatric concerns prior to their stroke. The purpose of this study was to capture the frequency of anxiety, depression, and PTSD in post-ischemic stroke patients. The results showed that 11% of the patients had developed post-stroke PTSD, 13% developed anxiety, and 20% developed depression. However, many patients had more than one of these symptoms, meaning these three symptoms likely have a relationship with each other. Regardless, anxiety, depression, and post-stroke PTSD are all common complications of a stroke39.
| PTSD symptoms | Stroke connections |
| Anxiety | ⇓, ⇑ |
| Depression | ⇓, ⇑ |
| Memory loss | ⇓, ⇑ |
| Poor emotional regulation | ⇓, ⇑ |
| Trouble thinking and forming clear thoughts | ⇓, ⇑ |
Some studies have been done on a more specific subject, such as how patients who have Transient Ischemic Attack (TIA) can develop post-TIA PTSD. A transient ischemic attack is a mini-stroke, wherein a person gets temporary symptoms of a stroke for a short period of time. A TIA is caused by blood clots, or fatty deposits, that decrease blood flow to a part of the brain. Unlike a stroke, though, a TIA does not cause permanent damage to any part of the brain. This specific study showed that 29.6% of the patients developed post-TIA PTSD. The study also reported that post-TIA patients who develop PTSD are also more likely to develop anxiety and depression as a result of their post-TIA PTSD (Table 2). One of the biggest symptoms or signs of post-TIA PTSD is poor coping strategies, for example, self-isolation or abusing substances. More research into post-TIA PTSD could be focused on education about proper coping strategies and what a transient ischemic attack is, as it is not well-known40. There was another study done on post-stroke and post-TIA patients. The goal of this study was, again, to see the prevalence of post-stroke/post-TIA PTSD in these patients. However, here researchers divided the patients into two groups: patients who had a stroke/TIA within a year and patients who had a stroke/TIA more than a year later. The results showed that 23% of post-stroke/post-TIA patients developed post-stroke/post-TIA PTSD within a year of their stroke/TIA. 11% of the post-stroke/post-TIA patients developed post-stroke/post-TIA PTSD more than a year after their stroke/TIA. This study demonstrates that about 1 in 4 post-stroke/post-TIA patients will develop PTSD symptoms within a year after their stroke/TIA. This is yet another reason why new screenings, preventatives, and treatments need to be developed for post-stroke/post-TIA patients, as it is clear that post-stroke/post-TIA PTSD develops quickly41. Another study was done on the relationship between stroke symptoms and PTSD in patients who had a TIA. The patients involved in this study self-reported symptoms of Acute Stress Disorder (ASD) as early as 3 days post-TIA. These patients also self-reported symptoms of PTSD as early as 1 month after they had their TIA. The results of this study showed that there was a positive relationship between TIA and ASD. The researchers believed that the combination of a TIA and ASD symptoms can develop into PTSD symptoms if the ASD symptoms are not recognized soon and there is no action taken on the ASD symptoms9.
| Stroke type | Associated PTSD risk |
| Ischemic Stroke | ⇓ |
| Hemorrhagic Stroke | ⇑ |
| Transient Ischemic Attack (TIA) | ⇓ |
Hemorrhagic Stroke and PTSD
Another study dives more into depth about how PTSD could cause a hemorrhagic stroke specifically. One of the ways to treat PTSD is through antidepressants, but antidepressants can also cause excessive bleeding, specifically a hemorrhagic stroke. In this study, there were over 1 million veterans examined for PTSD. Unsurprisingly, all of these veterans had developed PTSD. This study lasted 13 years, and all of these veterans made several visits on average every 2 years. The results showed that 507 of these patients suffered a hemorrhagic stroke. The factors that made any of these veterans more likely to have a hemorrhagic stroke were the following: PTSD, selective serotonin reuptake inhibitors (SSRIs), and selective norepinephrine reuptake inhibitors (SNRIs). PTSD was associated with an 82% greater risk of hemorrhagic stroke (Table 3). The use of SSRIs resulted in two-fold the risk of hemorrhagic stroke, and the use of SNRIs increased the risk for hemorrhagic stroke by 52%. So, between SSRIs and SNRIs, the safer option to treat PTSD is SNRIs because they have a lower risk of causing hemorrhagic stroke, whereas SSRIs have a very high risk of causing a hemorrhagic stroke. However, there have not been many studies focused on whether a hemorrhagic stroke specifically could cause PTSD. Ischemic strokes are more common than hemorrhagic strokes, and ischemic stroke has received the majority of the research focus in the past42.
Can PTSD Cause a Stroke?
The following studies provide support for the second question about the bidirectional relationship between a stroke and PTSD: “Does having PTSD make it more likely for a person to have a stroke?”. This first study involved patients who all survived 9/11. The purpose of this study was to determine if these patients, who experienced dust inhalation and have PTSD, would be at a higher risk for stroke. The results of this study showed that those with PTSD had a higher likelihood of developing an ischemic or hemorrhagic stroke(Table 3). However, those who inhaled large amounts of dust from 9/11 would be more at risk for hemorrhagic strokes specifically and recurring strokes as well43. Another study also examined whether having PTSD would make a person more likely to have a stroke. The patients involved in this study all have PTSD, no prior history of stroke, and are either 18 or older (n = 5,217). The rest of the participants in the study were part of the control group (n = 20,868).The results of this study showed that people who have PTSD are more likely to have a stroke, and are more likely to have an ischemic stroke than a hemorrhagic stroke (Table 2). However, many papers that have explored the topic of how PTSD affects stroke call for more research to be done to solidify the argument that PTSD can affect stroke44.
Another study discusses how PTSD can influence stroke risk factors and how PTSD can be an independent factor related to stroke. This paper divided its evidence into two categories: 1. How can PTSD influence stroke risk factors? and 2. How can PTSD be an independent factor that relates to stroke? This paper collected its evidence by indexing the literature to find that PTSD alone is related to several stroke risk factors and can also be an independent indicator of stroke (Table 2). The paper goes on to say that screening and identification of traumatic experiences would be helpful in getting stroke patients the psychological and physical help they need in order to reduce the risk of stroke significantly worldwide45.
Changes in Brain Morphology Due to PTSD
In general, PTSD is associated with structural, metabolic, and molecular changes in many regions of the brain. The areas of the brain that are typically impacted by PTSD are the amygdala, hippocampus, and prefrontal cortex, all of which are important for learning and storing memories. As shown in several studies, abnormalities in these regions of the brain in humans are a good indication of PTSD. The way doctors and scientists can identify PTSD in the brain, excluding other symptoms, is through neuroimaging. Over the past couple of years, neuroimaging has advanced to the point that it can be used to detect structural and metabolic changes in the brain. The specific brain scan that can do this is a Magnetic Resonance Imaging (MRI). MRIs will be able to detect the structural and metabolic changes in the human brain. This means MRIs have the capability to detect the early stages of PTSD since one of the ways of detecting PTSD is by catching physical abnormalities in the brain29. In another study, there were patients who had strokes and TIAs. The purpose of analyzing neuroimaging in this study was to see if brain scans would capture physical abnormalities in the brain that could be an indication for post-stroke, or even post-TIA, PTSD. The patients in this study underwent neuroimaging at the very beginning of the study and then went for visits 6, 12, and 24 months later. The results showed that 11% of the patients developed probable PTSD from their stroke or TIA. However, the study found that patients who had a stroke were more likely to develop PTSD than patients who had a TIA (Table 3). Stroke severity, large lesions, and reduced hippocampal activity made patients more prone to develop post-stroke/post-TIA PTSD. When it comes to coping mechanisms, the study found that high anxious and defensive coping styles made it more likely, and were signs of, for these patients to develop PTSD. However, the best way to prevent post-stroke/post-TIA is to identify and treat early on in post-stroke/post-TIA patients to prevent progression46.
MRI scans have also identified other regions of the brain, such as the prefrontal cortex and limbic system, that experience changes due to PTSD. Changes in brain morphology due to PTSD, as mentioned above, can lead to post-stroke PTSD. The brain regions affected by post-stroke PTSD are the limbic system (consists of the hypothalamus, thalamus, hippocampus, and amygdala) and the prefrontal cortex. Abnormalities in these parts of the brain can be a result of a person who is recovering from a stroke. As a result, these abnormalities cause these parts of the brain to function abnormally. Changes in brain morphology post-stroke are very important in order to track the relationship between a stroke and the potential presentation of post-stroke PTSD. These changes are indicators of early-stage post-stroke PTSD, or that post-stroke PTSD could manifest without treatment. So, changes in brain morphology can cause post-stroke PTSD, especially when the damage is associated with the limbic system and the prefrontal cortex. The limbic system and the prefrontal cortex are important for learning, memory storage, and emotional regulation. As these regions are involved in such vast functions, it is clear how harmful damage to the areas can be. Patients can experience difficulty learning, problems with speech (speaking or comprehension), short-term memory retention, regulation of emotions, etc. Most of these changes in behavior in people with damage to the limbic system and prefrontal cortex, due to stroke, are indicators of post-stroke PTSD47.
Importance of Community for Post-stroke Patients’ Recovery
As mentioned above, many factors contribute to a post-stroke patient’s recovery: medications, therapy, as well as a support system. Medications and therapy are what people think are the most important factors for any person going through the recovery stage after a life-altering injury. However, it is crucial not to overlook the importance of a support system when a patient is in recovery. It is true that medications and therapy greatly help a patient in their recovery process. But having a support system will provide mental stability for the patient recovering. This is very important because while the patient is recovering, the doctors and families do not want anything to go awry mentally. Having a support system can help with this goal.
One study examined how big a role caregivers had in the post-stroke patients’ recovery process. This study involved 26 stroke patients and 35 caregivers, all of whom were family. The main purpose of the caregivers in this study was that they were supposed to be multidimensional, meaning they played different roles in the post-stroke patient’s recovery to make the patient’s recovery easier. In this study, the caregivers were crucial in healthcare decision-making for these stroke survivors, who were not mentally and/or physically fit to make these decisions. There were two types of caregiver relationships in this study: adult-child type and spousal-type caregivers. The caregivers in an adult-child type relationship were engaged in being collaborative in decision-making with their patient(s). In contrast, the caregivers in a spousal-type relationship were more focused on making decisions for their partner, the patient, that would preserve their relationship. Their research recommended that best ways to create a capable and equipped caregiver for post-stroke patients are to give them the proper skillset to make decisions, provide a supportive decision-making environment, and reinforce communication with healthcare professionals and the patient to make the best decision possible48. Similarly, another study aimed to see how important it was for stroke survivors to have a community/support system around them while they were in the hospital, recovering, and when they were discharged from the hospital. This study took place under a German healthcare system, which has different rules and regulations as compared to those in the United States. In the German healthcare system, after patients are discharged from the hospital, there are no standard care programs for the patients. This leaves the patients responsible for their own care, according to their judgment, after they leave the hospital. This study included patients who had a stroke and a transient ischemic attack (TIA). There was a control group and an intervention group. The intervention group received care through the phone or face-to-face for up to a year after the start of the study. However, the control group received the standard German care. The results of the study showed that the patients who were part of the intervention group went to see their neurologists more often and were readmitted to the hospital less frequently. This caused the patients in the intervention group to not only save money on hospital visits but also confirm with multiple doctors that their healing process was progressing. This demonstrates how beneficial a support system is for post-stroke patients because if post-stroke patients have proper care, both mentally and physically, then they are likely to have a smoother and successful recovery compared to post-stroke patients who do not have an adequate support system around them49. Overall, through these studies, there is evidence that having a solid support system around post-stroke patients can lead to a more successful recovery process.
Through several studies, it has become apparent that if post-stroke patients have a community and/or support system around them during their recovery, then they are highly likely to have a more successful recovery than post-stroke patients who do not have a support system around them. This is because post-stroke patients not only have to heal physically, through medications and therapies, but they need to heal mentally as well. A support system allows post-stroke patients to know that they are not alone in their recovery journey as well. Having a support system will help the mental stability of a post-stroke patient greatly/
Therapeutics for Post-stroke PTSD
The ways to treat post-stroke PTSD are medications and therapies. As mentioned above, SSRIs and SNRIs are just one of the ways PTSD can be treated. However, the biggest side effect of using SSRIs and SNRIs is that they both increase the chances of having a hemorrhagic stroke, which can cause further post-stroke and regular PTSD (Table 3)42. However, there are other ways to treat post-stroke PTSD specifically. Repetitive transcranial magnetic stimulation (rTMS) is a type of rehabilitation method that can be used to treat post-stroke and regular PTSD. In one study, post-stroke patients, all of whom have post-stroke PTSD, received 10 sessions of rTMS treatment over the course of 2 weeks. There were PTSD tests before the treatment, one week into the treatment, and at the end of the treatment. There was also a 3-month follow-up visit to measure the PTSD symptoms again. The results showed that the repeated use of rTMS had decreased PTSD in these patients. However, this study suggests that rTMS should be coupled with other post-stroke therapies in order to see more significant results50. There are also psychological therapies used to treat post-stroke PTSD. In one study, the types of therapy used were preventive and supportive therapy. All the patients in this study had a stroke, either ischemic or hemorrhagic. Preventative therapy was used on a portion of the patients to prevent post-stroke PTSD, and regular counseling was used on the rest of the patients. Then, there was a 2-month follow-up visit. Any of the patients who developed post-stroke PTSD would then get supportive therapy to ease and hopefully treat the post-stroke PTSD, and the rest of the patients who did not develop post-stroke PTSD would get regular counseling. The results of this study showed that between the two therapies, supportive therapy was more successful in treating post-stroke PTSD than preventative therapy. However, the study reported that early supportive therapy for post-stroke patients would have the best outcomes19.
Another type of therapy used for treating post-stroke PTSD is Acceptance and Commitment Therapy (ACT). ACT is a type of psychotherapy that is used to help patients with post-stroke PTSD decrease their psychological inflexibility (PIF) and increase their psychological flexibility (PF) so that they can handle spontaneous and unavoidable situations. ACT is also a way to determine if a person is psychologically inflexible through six main categories: cognitive defusion (looking at thoughts rather than from them), acceptance, being present, values, committed action, and self as context. ACT is usually administered by a therapist who gives a patient scenarios/experiences and the patient would have to use their skillset from ACT to navigate through these scenarios51. One study conducted a trial to see whether ACT can decrease PIF and increase PF. This study consisted of 1,750 people, all of whom had a low PF and a high PIF. The results showed that ACT is a treatment option that is successful in increasing PF levels and decreasing PIF levels52. Another study aimed to see whether ACT could decrease PIF and increase PF as well. The findings showed that ACT can help improve PF and decrease PIF. In addition to increasing PF and decreasing PIF, ACT can also treat a variety of disorders such as psychosis, depression, obsessive-compulsive disorder (OCD), trichotillomania (an irresistible urge to pull out ones hair), anxiety disorders, and even PTSD/post-stroke PTSD. PIF has a strong association with PTSD in general, which can include post-stroke PTSD, meaning that PIF is an indicator of PTSD. If ACT can help improve PF and decrease PIF, then ACT can possibly prevent PTSD, and its symptoms, from manifesting in post-stroke patients and other people with disorders that can be treated with ACT51.
As mentioned before, several medications such as SSRIs, SNRIs, and antidepressants are used to treat post-stroke/post-TIA PTSD42. However, medications can also serve as traumatic reminders of patients’ stroke/TIA. Researchers studying this topic hypothesized that post-stroke patients would not want to take their post-stroke or post-TIA medications due to being reminded about the trauma they went through with their stroke/TIA. The patients involved in this study already had post-stroke/post-TIA PTSD, but the aim of this study was to see if taking post-stroke/post-TIA medications could elevate patients’ post-stroke/post-TIA PTSD. The patients in this study were asked a series of questions: 1. Did thinking about your stroke medications make you feel nervous or anxious? ; 2. Did thinking about your stroke medications make you think about your risk for future strokes? ; and 3. Did you skip or avoid taking your stroke medications so you would not have to think about your stroke? The results of this study showed that 11% of the patients have elevated post-stroke PTSD. These same patients were also more likely to answer “yes” to the 3 questions they were asked. Unsurprisingly, the elevated PTSD symptoms also brought up symptoms of anxiety and nervousness. This study showed that post-stroke/post-TIA medications can serve as traumatic reminders of a patient’s stroke, therefore, post-stroke patients are less inclined to take the medications. The overall results of this study showed that the elevated levels of post-stroke/post-TIA PTSD were due to the patients not taking their post-stroke/post-TIA medications53.
There are several different treatments and therapies used to treat post-stroke PTSD. One of them is repetitive transcranial magnetic stimulation (rTMS). rTMS is a rehabilitation method used to treat post-stroke PTSD. One study, mentioned above, found that their patients had responded well to rTMS and that rTMS was able to reduce the symptoms of post-stroke PTSD. So, rTMS is effective in treating post-stroke PTSD. Regardless, some studies have reported that rTMS should be coupled with other post-stroke treatments to reduce symptoms of post-stroke PTSD50. Another way to treat post-stroke PTSD is through different types of psychological therapies. The two most popular psychological therapies used to treat post-stroke PTSD are supportive and preventative therapy. In one study, supportive therapy was able to reduce and treat post-stroke PTSD. In this same study, preventative therapy was also used to treat post-stroke PTSD. Preventative therapy was used at the beginning of this study to see if it could prevent PTSD symptoms from developing in the early stages of recovery from a stroke. The results showed that supportive therapy was better at treating post-stroke PTSD than preventative therapy, but preventative therapy did help with reducing post-stroke PTSD symptoms. However, this study went on to mention that supportive therapy should be used in early post-op in post-stroke patients to maximize the effect of reducing post-stroke PTSD symptoms19. Furthermore, SSRIs and SNRIs are medications used to treat post-stroke PTSD, and they can also prevent early-stage symptoms of post-stroke PTSD from manifesting as well. The downside of using SSRIs and/or SNRIs is that they can also cause hemorrhagic strokes. This can lead to further damage to the brain regions and possibly a higher severity of post-stroke PTSD42. Out of all these potential treatments, rTMS is likely the best treatment, as it has little to no known side effects that could potentially harm patients using it.
On the other hand, post-stroke PTSD can be treated by coupling different types of therapies to maximize the desired result: reducing and/or preventing symptoms of post-stroke PTSD. The first proposition is to use supportive therapy and SSRIs/SNRIs together to treat post-stroke PTSD. Although SSRIs and SNRIs can cause hemorrhagic stroke, they are effective in treating post-stroke PTSD. Therefore, it makes sense to use SSRIs and SNRIs to treat post-stroke PTSD, but in moderation to avoid this risk. One treatment idea for post-stroke PTSD is to start off with supportive therapy to treat indicators of PTSD, so that these indicators do not fully develop into post-stroke PTSD. Then, after supportive therapy is used in the beginning, if some indicators of post-stroke PTSD are still lingering, patients can use SSRIs/SNRIs to eliminate the remaining symptoms. The supportive therapy goes in at the beginning of this course of treatment and does the grunt work of eradicating as many symptoms of post-stroke PTSD as possible. Then, if any symptoms persist, SSRIs and SNRIs can be used, hopefully for a short period of time, to reduce or eliminate any lingering symptoms. The important part of this course of treatment is that SSRIs and SNRIs will not have to be used for a long period of time, since most of the work to get rid of the symptoms was done via supportive therapy. This allows the SSRIs and SNRIs to be highly effective in getting rid of post-stroke PTSD symptoms without putting the patient at risk for a hemorrhagic stroke. The view behind this proposition is that supportive therapy should be able to get rid of the majority of the symptoms of post-stroke PTSD in the beginning, and the SSRIs and SNRIs would be used, for a short period of time, to eradicate any remaining symptoms of post-stroke PTSD should be successful. Another possibility of therapies that can be coupled together is preventative therapy and rTMS. This treatment plan can start off with preventative therapy, which has been shown to reduce post-stroke PTSD symptoms, and can be used aggressively to reduce post-stroke PTSD symptoms. The second step in this treatment plan would be to use rTMS, which would be a rehabilitation-style approach to eliminate any remaining symptoms of post-stroke PTSD. Between these two types of treatments, rTMS is less aggressive; therefore, it would be favorable to end a treatment plan and a good option to contrast with the aggressive preventative therapy. The thought process with this treatment plan is to start off aggressively with preventative therapy and end with a rehabilitative-style treatment such as rTMS.
Overall, post-stroke PTSD and PTSD in general are hard to spot and diagnose in their early stages due to much-needed technological advancements. Therefore, there are not many treatment options, as of right now, that are successful in treating post-stroke PTSD. The treatments mentioned above have been researched the most, and have worked with many patients; therefore, they are part of the very few treatments used to treat post-stroke PTSD.
Proposals for Gaps in Literature
The topics of stroke and PTSD are being heavily researched to this day because there is still a lot of information that is unknown to researchers in these areas. Specifically with stroke, researchers should focus more on the complications of stroke, such as post-stroke seizures, post-stroke PTSD, etc., rather than on how to prevent it. In contrast, with PTSD, researchers should focus on the indicators and factors of PTSD, such as anxiety, depression, personality disorders, etc., rather than PTSD as a whole.
Firstly, with stroke, one study aimed to see whether anti-epileptic drugs (AEDs), such as diazepam, and primary prophylaxis could prevent post-stroke seizures in post-stroke patients. As mentioned before, seizures in post-stroke patients are one of the most fatal risks during recovery. Several studies before this specific one have concluded that diazepam might help prevent post-stroke seizures. However, these same studies have reported that more research needs to be done in order to prove this statement to be true. In this study, a total of 856 post-stroke patients were involved. The study divided these patients into two groups: post-stroke patients with no seizures and post-stroke patients with at least 1 seizure post-stroke. The results of this study showed that when diazepam and primary prophylaxis were used individually, there was not any concrete evidence to show that either of them was able to decrease the risk of post-stroke seizures. However, this study also concluded that when diazepam and primary prophylaxis were used together, they were both beneficial in reducing the chances of post-stroke seizure in post-stroke patients54. This study has moved closer to answering the following question: Can AEDs, such as diazepam, be effective in reducing the risk for post-stroke seizures in post-stroke patients? Furthermore, this study has called for more research to be done in order to prove this question to be true. One research proposal for this field of study could start by gathering post-stroke patients, all of whom have had at least 2 seizures post-stroke. The requirements for the people involved in this study would be that they have to have had their stroke more than 5 years ago, with at least 2 or more seizures happening post-stroke. Then, the people involved in this study would be separated into two groups: the control group (the group that will not receive diazepam as a treatment for their seizures) and the intervention group (the group that will receive diazepam as a treatment for their seizures). For the intervention group, the patients will get their diazepam via IVs once a week for 6 weeks. Based on the previous studies on the effectiveness of diazepam, the outcome would hopefully be that the participants have enough diazepam in their bodies to prevent post-stroke seizures for a long period of time.
Moving ahead, there needs to be additional studies done on how effective Acceptance and Commitment Therapy (ACT) is in decreasing the symptoms of PTSD and to what extent ACT can be utilized to improve other disorders. As mentioned above, ACT is a type of psychotherapy that can be used to increase psychological flexibility (PF) and decrease psychological inflexibility (PIF). PIF is an indicator of PTSD; therefore, ACT can help in preventing PTSD or reducing the severity of PTSD in patients51. Some of the papers that have researched ACT have reported that although their research has shown ACT can decrease PIF, and by correlation decrease PTSD severity, more research is needed to solidify this argument. One research suggestion is the following: researchers can conduct a study that includes patients with low PF and high PIF in order to see how effective ACT is in decreasing PIF and increasing PF. These patients will be separated into two groups: the control group (will not receive ACT) and the intervention group (will receive ACT). The ACT will be administered on a weekly basis to the intervention group, and there will be follow-up visits every 2 weeks for 12 months. The trial will last 12 months so that there is adequate time given for the ACT to have an effect on decreasing the PIF and increasing the PF. Given the results of previous studies on ACT, it is hypothesized that through this research proposal, ACT will diminish PIF and, by association, PTSD, and increase PF.
In addition to the research proposals above, many researchers have called for more studies on how PTSD affects stroke and its risk factors. As mentioned above, it is easier to research PTSD when it is researched by its symptoms/indicators rather than as a whole. The symptoms of PTSD are the following: anxiety disorders, depression, personality disorders, etc. These symptoms of PTSD are all related to stroke in one way or another (Table 2). PTSD is commonly characterized by emotional shifts (depression and personality disorders) as a result of the trauma (anxiety disorders). One proposition of a study or trial for this topic could be to gather people who are eligible for this study. The requirements would be the following: people who have had PTSD for more than 5 years and people who do not have PTSD. Next, the participants could be divided into two groups: the control group (people with no PTSD) and the PTSD group (people who have had PTSD for more than 5 years). The next step would be to acquire brain scans on both the control and PTSD groups. Then, those scans could be analyzed to capture differences in activation patterns across the brain. While the participants undergo their MRIs, they will simultaneously go through visual, auditory, and olfactory stressors. Examples of these stressors are the following: pictures, sounds of guns explosions, planes, etc., and odors linked to trauma. In the brain scans of both groups, the researchers should pay close attention to the limbic system, which consists of the hypothalamus, thalamus, hippocampus, and amygdala. The limbic system is responsible for emotional regulation. So, the limbic system would look different in people with PTSD (symptoms of anxiety, depression, personality disorders, etc.) than in people who do not have PTSD. Based on previous studies, the people with PTSD in this research proposal should have an abnormal limbic system, whether one part is abnormal or the whole limbic system is abnormal, due to the trauma they have endured. The abnormalities in the limbic system would potentially show up on the brain scans. The researchers should be able to see that the people in the PTSD group have abnormal limbic systems compared to the people in the control group. The purpose of using visual, auditory, and olfactory stressors on the participants is to see the individuals’ responses as well as how one’s response affects their brain scans. Since several studies have found that there are positive associations between the symptoms of PTSD and the symptoms of stroke, the people in the PTSD group in this proposed study would have symptoms that have positive correlations with stroke and its symptoms (Tables 1 and 2). The purpose of this proposed trial is to utilize the symptoms of PTSD and the changes in the brain due to PTSD, to see how they affect the risk factors and/or symptoms of stroke.
Discussion and Future Directions
As mentioned above, many researchers have investigated the bidirectional relationship between stroke and post-traumatic stress disorder (PTSD). Many researchers predicted that having a stroke could make one more prone to developing PTSD, and vice versa, and the data was able to support these two hypotheses55. Many hypotheses were debated regarding the treatments that could be used to treat the general complications of a stroke56. Other hypotheses were debating the reliable treatments for stroke, PTSD, and post-stroke PTSD. The studies found that there are only a few reliable therapeutics and treatments that can be used for these illnesses. Some studies hypothesized that there would be a variety of medications used for treating post-stroke PTSD, when in reality, there were very few medications that were tested and allowed to be used to treat post-stroke PTSD57. In contrast, there were very few hypotheses debating the therapeutics used to treat PTSD58. This is because there is already awareness and research that has shown the valid therapies that can be used to treat PTSD. Once a diagnosis has been made, another tool that could be used to characterize the brains of those with PTSD is advanced screenings. As of right now, MRIs are one of the best ways to detect abnormal brain morphology, which is associated with PTSD46. However, some of the studies discussing stroke and PTSD have a small sample of people who participate in these studies, meaning the results might be broader or have more variation. One reason some studies have a small number of participants is that any history of illness makes it harder for many people to match the qualifications to participate in these studies. The biggest limitation of any study researching stroke and PTSD is the technology available to conduct the studies. Many studies that have obtained their results have also emphasized that there needs to be a development of technology to thoroughly study both stroke and PTSD complications. The only way, though, to be able to further develop technology for these respective topics is for there to be many more studies done on both of them.
One way to be able to treat post-stroke PTSD better is if doctors can catch it in its early stages. The only way to be able to do this is if there is an advancement in technology, specifically, in screenings and imaging. If there were more advanced screening, then it would be possible to detect abnormal brain morphology earlier in post-stroke patients or in a less invasive way46. Two of the medications used to treat post-stroke PTSD are selective serotonin reuptake inhibitors (SSRIs) and selective norepinephrine reuptake inhibitors (SNRIs). SSRIs and SNRIs work very well when it comes to treating post-stroke PTSD, but they can also lead to a hemorrhagic stroke42. As for therapies, there are psychological and repetitive transcranial magnetic stimulation (rTMS) therapies. Both of these therapies aim to prevent and treat post-stroke PTSD58. One direction any type of medical advancements should go in is in the post-stroke area. Instead of putting post-stroke patients, who have post-stroke PTSD, into many different types of therapies, there should be medical advancements when it comes to post-stroke medications. Post-stroke medications, and medications in general, are easier to take and are an option far less time-consuming than therapy. In the future, there needs to be an advancement in the technology used to detect abnormal brain morphology. This should be an advancement of the machines used for brain imaging, screenings, etc. MRIs are the best way, as of right now, to detect abnormal brain morphology46. In the future, there needs to be further advancement of the technology used for brain scans in order to catch, prevent, and treat post-stroke PTSD. Overall, there is certainly room for development when it comes to identifying and treating stroke, PTSD, and post-stroke PTSD.
The biggest advantage to have when it comes to treating stroke and its complications is time. The more time you have, the more options (i.e. therapies, medications, brain scans) that are available for treating post-stroke complications, such as post-stroke PTSD. In the future, the trajectory of therapies could be adjusted to specific post-stroke patients. Another approach is utilizing brain scans, such as MRIs, as a diagnostic tool for post-stroke patients with complications such as post-stroke PTSD. MRIs could also be used more frequently on post-stroke patients to not only track a patient’s progress in their recovery but also as a way for doctors to gather data on how effective certain post-stroke therapies are. Using MRIs more often can also allow doctors to correlate specific symptoms, in post-stroke patients, to which therapies are the most successful for these symptoms. Another factor in determining how well a post-stroke patient’s recovery goes is whether they have a support system or a community around them. A support system is crucial for the recovery phase because it can prevent the patient’s mental health from declining, as recovery is a daunting bridge to cross in order to become healthy and well again. However, there are many post-stroke patients who go through the recovery journey by themselves as they do not have a proper support system, therefore their recovery might be more difficult or slower. One treatment to consider for patients in this situation is to provide them with physical therapy (PT) or general therapy, which can act as a support system for lonely patients. This therapeutic support system can create a sense of community and potentially prevent the patient from further mental suffering and increase health outcomes.
Overall, researchers have attempted to cover the many factors associated with the bidirectional relationship between stroke and PTSD. However, many studies have made it clear that more research needs to be conducted in order to get to the crux of preventatives, treatments, therapies, etc. that can be used to combat both of these conditions. All things considered, many studies have begun to show results to indicate the following questions as truthful: “Can having a stroke make a person more likely to develop PTSD?” and “Does PTSD make it more likely for a person to have a stroke?”.
Methods
Several databases were searched, including PubMed and the National Library of Medicine, to retrieve information relevant to this literature review’s topics (Figure 1). The databases PubMed (records identified, n = 41) and the National Library of Medicine (records identified, n = 6) include randomized trials and systematic reviews. The reference lists in several of the papers used were also checked. A comprehensive summary of all references is provided below (Table 4). Searches for articles were also conducted on the internet; some of the references were from respectable websites and books as well. The main keywords that were used to conduct searches for articles were the following: stroke, post-traumatic stress disorder (PTSD), ischemic stroke, hemorrhagic stroke, and post-stroke PTSD.
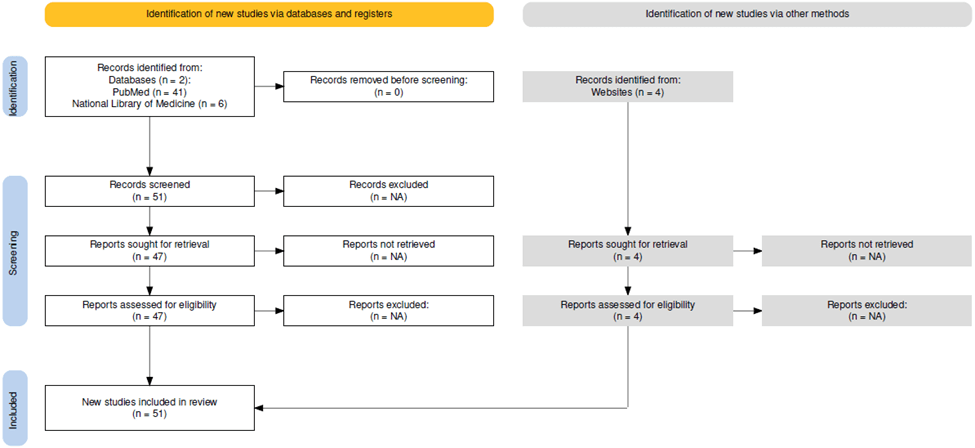
| Table 4: Summaries of Referenced Studies | ||||||
| Name of study | Authors | Year of publication | Method | Findings | Variables | Sample size |
| Posttraumatic Stress Symptoms After Stroke: The Effects of Anatomy and Coping Style | Assayag et. al, 202246 | 2022 | All participants went through MRIs and were examined 6, 12, and 24 months after the MRIs. | Post-stroke PTSD risk can be influenced by stroke location, severity, and future coping mechanisms | PTSD, symptoms, post-stroke | 436 |
| Effect of Water exercise Therapy on Lower Limb Function Rehabilitation in Hemiplegic Patients with the First Stroke | Bei et, al.15 | 2023 | Patients received rehabilitation treatment and were split into a control group and a hydrotherapy group | Early water exercise therapy intervention is most efficacious for first-time stroke survivors | Rehabilitation, water exercises, first stroke only. | 160 |
| What is the Fight, Flight, Freeze, or Fawn Response? | Cleveland Clinic59 | 2024 | Information about stress responses. | Outlines stress management and trauma prevention | N/A | N/A |
| How many people are affected by/at risk for stroke? | Office of Communications13 | 2022 | Information about different risks for stroke. | Influences of stroke | N/A | N/A |
| Community care coordination for stroke survivors: results of a complex intervention study | Johannes Deutschbein, Ulrike Grittner, Alice Schneider, Liane Schenk49 | 2020 | Care through telephone or face-to-face. A control group receiving standard care. | Care coordination is crucial for stroke survivor recovery. | Survivor of stroke/TIA, care coordination, costs, Germany, Health care utilization, readmissions, stroke. | 361 |
| Incidence, Implications, and Management of Seizures Following Ischemic and Hemorrhagic Stroke | Doria et, al.60 | 2019 | N/A | Incidence of post-stroke seizure and treatment outcomes. | Treatment of seizures, ischemic stroke, hemorrhagic stroke. | N/A |
| [Acceptance and commitment therapy] | D Ducasse, G Fond51 | 2015 | Systematic review/meta-analysis | ACT is a multi-use as it can treat a variety of disorders. | Acceptance and commitment therapy, randomized controlled trial. | 40 articles |
| Prevalence of PTSD in Survivors of Stroke and Transient Ischemic Attack | Edmondson et, al.41 | 2013 | Examined patients who had a stroke/TIA after ≥ one year. | 1 in 4 post-stroke patients will develop rapid-onset PTSD symptoms | Stroke, transient ischemic attack. | 1,138 |
| Acute stress symptoms 1-2 weeks after stroke predict the subsequent development of post-traumatic stress symptoms: A prospective cohort study | Feely et, al.61 | 2023 | Measuring of ASD 1-2 weeks (time 1) and then 6-12 weeks (time 2) later. | Early intervention for those showing post-stroke ASD results in better treatment outcomes. | Stroke severity, functional impairment, cognitive impairment, depression, anxiety, premorbid intelligence, and pain between the 2 time points. | 54 |
| Stroke facts & statistics | Stroke Awareness Foundation62 | 2023 | Information about stroke in general | Outlines stroke types and associated statistics | Ischemic stroke and hemorrhagic stroke | N/A |
| Posttraumatic Stress Disorder, Antidepressant Use, and Hemorrhagic Stroke in Young Men and Women: A 13-year Cohort Study | Gaffey et, al.42 | 2021 | Examined effects of PTSD, use of SSRIs & SNRIs, and stroke risk as a result through Cox models. | SNRIs are effective for treating PTSD and comorbidities | Hemorrhagic stroke, SSRIs, SNRIs, PTSD, Cox models, demographics, psychiatric comorbidities | 1,100,000 |
| Correlates of Post-traumatic Stress Disorder in Stroke Survivors | Goldfinger et, al.34 | 2014 | Measured prevalence of stroke-induced PTSD through the PTSD Checklist Specific for stroke (PCL-S) | Stroke-induced PTSD is associated with young age, recurrent stroke, disabilities, and comorbidities | Stroke-induced PTSD, TIA, PCL-S greater than 50, demographics, stroke history, disability, medical comorbidities, depression, and emotional support | 535 |
| Evidence of the dissociative PTSD subtype: A systematic literature review of latent class and profile analytic studies of PTSD | Maj Hansen, Jana Ross, Cherie Armour.63 | 2017 | Systematic review paper; six databases were used to collect information for this literature review | Evidence advocating for D-PTSD subtype classification | D-PTSD, PubMed, Web of Science, Scopus, PILOTSD, PsychInfo, and Embase | N/A |
| The effect of acceptance and commitment therapy on the psychological flexibility and inflexibility of undergraduate students: A systematic review and three-level meta-analysis | Ti Hsu, Jenna L. Adamowicz, Emily B K Thomas.52 | 2023 | Meta-analysis/systematic review: Information from 20 studies was used in the systematic review | ACT is an efficacious intervention as it relates to psychological flexibility | N/A | 1,750 |
| Supportive psychological therapy can effectively treat post-stroke post-traumatic stress disorder at the early stage | Jiang et, al.19 | 2022 | Randomized psycho-therapy vs control groups at 2 time points | Early supportive therapy was effective for positive post-stroke PTSD outcomes | Post-stroke PTSD | 170 |
| Effectiveness of repetitive transcranial magnetic stimulation combined with a brief exposure procedure for post-stroke posttraumatic stress disorder | Jiang et, al.50 | 2023 | Participants were randomly assigned to 3 groups, and after treatment, they had short-term and long-term evaluations. | rTMS and brief exposure therapy yield the best outcomes for post-stroke PTSD patients | rTMS and post-stroke PTSD | 60 |
| Medical complications and outcome after endovascular therapy for acute ischemic stroke | Junttola et, al.14 | 2021 | A retrospective singular-center study of patients who received EVT. | Avoiding medical complications during EVT is crucial to patient health | Pneumonia, acute cardiac insufficiency, and myocardial infarction | 380 |
| Examining posttraumatic stress disorder as a key postinjury risk factor in OIF/OEF veterans with blad-induced mild traumatic brain injury | Kim et, al.37 | 2020 | Included 3 groups: healthy controls, PTSD only, and comorbid blast-induced MTBI and PTSD. | The discrepancy in PS between the healthy controls and the comorbid group is due to PTSD and not to mTBI. | Perceived cognitive complications (PCC), perceived emotional distress (PED), and processing speed (PS) | 138 |
| Increased prevalence of posttraumatic stress disorder in patients after transient ischemic attack | Kiphuth et, al.40 | 2014 | Patients with TIA were studied and assessed after 3 months | TIA increases the risk for PTSD, anxiety, and depression | TIA, PTSD, anxiety, depression, and maladaptive coping strategies | 108 |
| Constraint-induced movement therapy after stroke | Kwakkel et, al.17 | 2015 | N/A | CIMT helps post-stroke patients improve upper limb mobility | Constraint-induced movement therapy (CIMT) | N/A |
| Socioeconomic status and stroke severity: Understanding indirect effects via risk factors and stroke prevention using innovative statistical methods for mediation analysis | Anite Lindmark, Marie Eriksson, and David Darehed6 | 2022 | Analysis of data collected through the Longitudinal integrated database for health insurance and labor market studies (LISA). | Low education level increased the chances for stroke | Ischemic stroke, socioeconomic status, and stroke | 86,316 |
| Medications as Traumatic Reminders in Patients with Stroke/Transient Ischemic Attack-Induced Posttraumatic Stress Disorder | Jiang et, al.19 | 2021 | Patients with a suspected stroke/TIA were evaluated post-hospitalization | Medications can serve as a traumatic reminder of post-stroke/post-TIA PTSD | Post-stroke, post-TIA, and PTSD. | 408 |
| Psychological inflexibility predicts PTSD symptom severity in war veterans after accounting for established PTSD risk factors and personality | Meyer et, al.36 | 2019 | 1-year psychological follow-up in Iraq and Afghanistan veterans | Psychological inflexibility and PTSD symptoms severity are associated | Psychological inflexibility, PTSD, and veterans | 236 |
| Meta-Analysis of Cultural Influences in Trauma Exposure and PTSD Prevalence Rates | Linda Denise Oakley, Wan-Chin Kuo, Jennifer A Kowalkowski, and Wanju Park30 | 2021 | Meta-analysis of factors associated with PTSD | Refugees displaced in similar cultures had higher rates of PTSD | PTSD, culture, gender, refugees, and trauma. | 3,403 |
| Relationship between NIH stroke symptoms and post-traumatic stress disorder in patients evaluated for transient ischemic attack/stroke | Pedowitz et, al.9 | 2021 | Patients self-reported ASD symptoms post-stroke/post-TIA shortly after then after 1 month; stroke symptoms were evaluated prior to hospital discharge. | Stroke disability is positively associated with ASD and PTSD symptoms early in recovery | Post-stroke, post-TIA, PTSD, and ASD | 300 |
| Prevalence and correlates of post-traumatic stress disorder after ischaemic stroke | Rutovic et, al.38 | 2021 | PCL-S was used to diagnose PTSD, HADS was used to assess depression and anxiety, and stroke severity was assessed using mRS | PTSD and disability severity are positively correlated | Ischemic stroke, PTSD, and brain regions | 85 |
| Prevalence of post-traumatic stress disorder in the United States: a systematic literature review | Schein et, al.31 | 2021 | Systematic literature review: articles from MEDLINE, EMBASE, and PsycINFO were used | Prevalence of PTSD was elevated in vulnerable populations and minorities | Post-traumatic stress disorder, prevalence, risk factors, and systematic literature review | N/A |
| Stroke Neurology | Michael Schneck, Karen Orjuela, and Clio Rubinos64 | 2016 | Book | An introduction to the basics of stroke. | Stroke, ischemic stroke, and hemorrhagic stroke | N/A |
| Association Between Anxiety, Depression, and Post-traumatic Stress Disorder and Outcomes After Ischemic Stroke | Stein et, al.39 | 2018 | A telephone survey was conducted to assess depression, anxiety, and PTSD 6-12 months after ischemic stroke | Anxiety, depression, and PTSD are common post-stroke complications and have high rates of co-occurrence | Ischemic stroke, anxiety, depression, and PTSD. | 55 |
| Post-Traumatic Stress Disorder After Stroke | Tang et, al.33 | 2022 | Systematic review: PubMed, EMBASE, PsycINFO, and Ovid Nursing were searched for studies related to post-stroke PTSD | Results showed that PTSD is common post-stroke. | Stroke and PTSD | 1,785 |
| Treatment with Diazepam in Acute Stroke Prevents Postsroke Seizures: A Substudy of the EGASIS Trial | van Tuijl et, al.16 | 2022 | Acute stroke patients were treated with diazepam or placebo for 3 days; follow-ups were 2 weeks and 3 months later | Diazepam was effective in preventing seizures in the first 3 months following stroke | Post-stroke seizures and diazepam | 784 |
| Seeking healthcare services post-stroke: a qualitative descriptive study exploring family caregiver and stroke survivor perspectives in an asian setting | Tyagi et, al.48 | 2021 | Interviews with stroke survivors and family caregivers | Caregivers have multidimensional roles in caring for stroke survivors | Stroke, healthcare, and caregivers | 61 |
| Posttraumatic Stress Disorder and Anxiety-Related Conditions | John B. Williamson, Michael S. Jaffee, and Ricardo E. Jorge21 | 2021 | Synopsis of current treatments and assessments for PTSD and anxiety disorders. | PTSD is more related to trauma than to anxiety disorders | PTSD, treatments, and anxiety disorders | N/A |
| Neurobiological and genetic correlates of the dissociative subtype of posttraumatic stress disorder | Wolf et, al.65 | 2023 | Psychological, neuroimaging, and biomarker assessments in post-9/11 veterans | Biological structures, neural representation, spatial awareness, and spatial learning and memory are positively associated with D-PTSD. | Dissociated PTSD, neuroimaging, and biomarkers | 374 |
| Stroke hospitalizations, posttraumatic stress disorder, and 9/11-related dust exposure: Results from the World Trade Center Health Registry | Yu et, al.43 | 2021 | Stroke cases were obtained through the World Trade Center Health Registry | PTSD is a risk factor for ischemic and hemorrhagic stroke | 9/11, stroke, hospitalization, and PTSD | 29,012 |
References
- Foundation, S. awareness. (2023, July 11). Stroke facts & statistics. Stroke Awareness Foundation. https://www.strokeinfo.org/stroke-facts-statistics/#:~:text=Someone%20has%20a%20strke%20every,disability%20in%20the%20United%20States. [↩]
- Schneck M, & Orjuela K, & Rubinos C (2016). Stroke neurology. Salardini A, & Biller J(Eds.), The HospitalNeurology Book. McGraw-Hill Education. https://neurology.mhmedical.com/content.aspx?bookid=1779§ionid=122853486 [↩]
- Brown, R. D. (2024, April 30). Stroke. Mayo Clinic. https://www.mayoclinic.org/diseasesonditions/stroke/symptoms-causes/syc-20350113 [↩]
- R. D. (2024, April 30). Stroke. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/stroke/symptoms-causes/syc-20350113 [↩]
- Brown, R. D. (2024, April 30). Stroke. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/stroke/symptoms-causes/syc-20350113 [↩] [↩] [↩] [↩]
- Lindmark A, Eriksson M, Darehed D. Socioeconomic status and stroke severity: Understanding indirect effects via risk factors and stroke prevention using innovative statistical methods for mediation analysis. PLoS One. 2022 Jun 24;17(6):e0270533. Doi: 10.1371/journal.pone.0270533. PMID: 35749530; PMCID: PMC9232158. [↩] [↩]
- Lindmark A, Eriksson M, Darehed D. Socioeconomic status and stroke severity: Understanding indirect effects via risk factors and stroke prevention using innovative statistical methods for mediation analysis. PLoS One. 2022 Jun 24;17(6):e0270533. Doi:
10.1371/journal.pone.0270533. PMID: 35749530; PMCID: PMC9232158. [↩]
- Marshall IJ, Wang Y, Crichton S, McKevitt C, Rudd AG, Wolfe CD. The effects of socioeconomic status on stroke risk and outcomes. Lancet Neurol. 2015
Dec;14(12):1206-18. doi: 10.1016/S1474-4422(15)00200-8. PMID: 26581971. [↩]
- Pedowitz E, Derby L, Cruz GJ, Trainor A, Edmondson D, Cornelius T. Relationship between NIH stroke symptoms and post-traumatic stress disorder in patients evaluated for transient ischemic attack/stroke. Gen Hosp Psychiatry. 2021 May-Jun;70:98-102. Doi: 10.1016/j.genhosppsych.2021.03.004. Epub 2021 Mar 8. PMID: 33774490; PMCID: PMC8127400. [↩] [↩] [↩]
- Schwarzbach CJ, Grau AJ. Komplikationen nach Schlaganfall : Klinische Herausforderungen in der Schlaganfallnachsorge [Complications after stroke : Clinical challenges in stroke aftercare]. Nervenarzt. 2020 Oct;91(10):920-925. German. doi: 10.1007/s00115-020-00988-9. PMID: 32914296. [↩]
- Schwarzbach CJ, Grau AJ. Komplikationen nach Schlaganfall : Klinische Herausforderungen in der Schlaganfallnachsorge [Complications after stroke : Clinical challenges in stroke aftercare]. Nervenarzt. 2020 Oct;91(10):920-925. German. doi: 10.1007/s00115-020-00988-9. PMID: 32914296. [↩]
- Doria JW, Forgacs PB. Incidence, Implications, and Management of Seizures FollowingIschemic and Hemorrhagic Stroke. Curr Neurol Neurosci Rep. 2019 May 27;19(7):37. doi: 10.1007/s11910-019-0957-4. PMID: 31134438; PMCID: PMC6746168. [↩]
- Communications, O. of. (2022). How many people are affected by/at risk for stroke?. Eunice Kennedy Shriver [↩] [↩]
- Junttola U, Lahtinen S, Liisanantti J, Vakkala M, Kaakinen T, Isokangas JM. Medical complications and outcome after endovascular therapy for acute ischemic stroke. Acta Neurol Scand. 2021 Dec;144(6):623-631. Doi: 10.1111/ane.13501. Epub 2021 Jul 14. PMID: 34263446. [↩] [↩]
- Bei N, Long D, Bei Z, Chen Y, Chen Z, Xing Z. Effect of Water Exercise Therapy on Lower Limb Function Rehabilitation in Hemiplegic Patients with the First Stroke. Altern Ther Health Med. 2023 Oct;29(7):429-433. PMID: 37573592. [↩] [↩]
- van Tuijl JH, van Raak EPM, van Oostenbrugge RJ, Aldenkamp AP, Rouhl RPW. Treatment with Diazepam in Acute Stroke Prevents Poststroke Seizures: A Substudy of the EGASIS Trial. Cerebrovasc Dis. 2021;50(2):216-221. doi: 10.1159/000512799. Epub 2021 Jan 19. PMID: 33465768. [↩] [↩]
- Kwakkel G, Veerbeek JM, van Wegen EE, Wolf SL. Constraint-induced movement therapy after stroke. Lancet Neurol. 2015 Feb;14(2):224-34. doi: 10.1016/S1474-4422(14)70160-7. PMID: 25772900; PMCID: PMC4361809. [↩] [↩]
- El Husseini N, Katzan IL, Rost NS, Blake ML, Byun E, Pendlebury ST, Aparicio HJ, Marquine MJ, Gottesman RF, Smith EE; American Heart Association Stroke Council; Council on Cardiovascular and Stroke Nursing; Council on Cardiovascular Radiology and Intervention; Council on Hypertension; and Council on Lifestyle and Cardiometabolic Health. Cognitive Impairment After Ischemic and Hemorrhagic Stroke: A Scientific Statement From the American Heart Association/American Stroke Association. Stroke. 2023 Jun;54(6):e272-e291. doi: 10.1161/STR.0000000000000430. Epub 2023 May 1. PMID: 37125534. [↩]
- Jiang C, Li Z, Du C, Zhang X, Chen Z, Luo G, Wu X, Wang J, Cai Y, Zhao G, Bai H. Supportive psychological therapy can effectively treat post-stroke post-traumatic stress disorder at the early stage. Front Neurosci. 2022 Oct 6;16:1007571. Doi: 10.3389/fnins.2022.1007571. PMID: 36278005; PMCID: PMC9583431. [↩] [↩] [↩] [↩] [↩] [↩]
- Jakšić N, Brajković L, Ivezić E, Topić R, Jakovljević M. The role of personality traits in posttraumatic stress disorder (PTSD). Psychiatr Danub. 2012 Sep;24(3):256-66. PMID: 23013628. [↩] [↩] [↩]
- Williamson JB, Jaffee MS, Jorge RE. Posttraumatic Stress Disorder and Anxiety-Related Conditions. Continuum (Minneap Minn). 2021 Dec 1;27(6):1738-1763. doi: 10.1212/CON.0000000000001054. PMID: 34881734. [↩] [↩] [↩] [↩] [↩]
- Clinic, C. (2024, July 22). What happens during fight-or-flight response?. Cleveland Clinic. https://health.clevelandclinic.org/what-happens-to-your-body-during-the-fight-or-flight-rsponse [↩]
- Kramer A, Kovach S, Wilkins S. An Integrative Review of Behavioral Disturbances in Veterans With Dementia and PTSD. J Geriatr Psychiatry Neurol. 2022 May;35(3):262-270. Doi: 10.1177/0891988721993572. Epub 2021 Feb 19. PMID: 33601943. [↩] [↩]
- Asmundson GJ, Stapleton JA, Taylor S. Are avoidance and numbing distinct PTSD symptom clusters? J Trauma Stress. 2004 Dec;17(6):467-75. doi: 10.1007/s10960-004-5795-7. PMID: 15730065. [↩]
- Weathers, F.W., Blake, D.D., Schnurr, P.P., Kaloupek, D.G., Marx, B.P., & Keane, T.M. (2013). The Clinician-Administered PTSD Scale for DSM-5 (CAPS-5). [Assessment] [↩]
- Flood AM, Boyle SH, Calhoun PS, Dennis MF, Barefoot JC, Moore SD, Beckham JC. Prospective study of externalizing and internalizing subtypes of posttraumatic stress disorder and their relationship to mortality among Vietnam veterans. Compr Psychiatry. 2010 May-Jun;51(3):236-42. Doi: 10.1016/j.comppsych.2009.08.002. PMID: 20399332; PMCID: PMC2858053. [↩]
- Wolf EJ, Hawn SE, Sullivan DR, Miller MW, Sanborn V, Brown E, Neale Z, Fein- Schaffer D, Zhao X, Logue MW, Fortier CB, McGlinchey RE, Milberg WP. Neurobiological and genetic correlates of the dissociative subtype of posttraumatic stress disorder. J Psychopathol Clin Sci. 2023 May;132(4):409-427. doi: 10.1037/abn0000795. Epub 2023 Apr 6. PMID: 37023279; PMCID: PMC10286858.; Hansen M, Ross J, Armour C. Evidence of the dissociative PTSD subtype: A systematic literature review of latent class and profile analytic studies of PTSD. J Affect Disord. 2017 Apr 15;213:59-69. Doi: 10.1016/j.jad.2017.02.004. Epub 2017 Feb 7. PMID: 28192736. [↩]
- Stein MB, Hanna C, Koverola C, Torchia M, McClarty B. Structural brain changes in PTSD. Does trauma alter neuroanatomy? Ann N Y Acad Sci. 1997 Jun 21;821:76-82. Doi: 10.1111/j.1749-6632.1997.tb48270.x. PMID: 9238195.; Kuznetsov A, Kokorev D, Sustretov A, Kozlov A, Lyamin A, Sheyfer M, Kolsanov A, DeSousa A, Cumming P, Gayduk A. Genetic Contributors to PTSD: the Role of SNVs, Gene Interactions and Haplotypes for Developing PTSD Prevention Measures. A Comprehensive Review. Psychiatr Danub. 2023 Oct;35(Suppl 2):141-149. PMID: 37800217. [↩]
- Nisar S, Bhat AA, Hashem S, Syed N, Yadav SK, Uddin S, Fakhro K, Bagga P, Thompson P, Reddy R, Frenneaux MP, Haris M. Genetic and Neuroimaging Approaches to Understanding Post-Traumatic Stress Disorder. Int J Mol Sci. 2020 Jun 4;21(12):4503. doi: 10.3390/ijms21124503. PMID: 32599917; PMCID: PMC7352752. [↩] [↩]
- Oakley LD, Kuo WC, Kowalkowski JA, Park W. Meta-Analysis of Cultural Influences in Trauma Exposure and PTSD Prevalence Rates. J Transcult Nurs. 2021 Jul;32(4):412-424. doi: 10.1177/1043659621993909. Epub 2021 Feb 16. PMID: 33593236. [↩] [↩]
- Schein J, Houle C, Urganus A, Cloutier M, Patterson-Lomba O, Wang Y, King S, Levinson W, Guérin A, Lefebvre P, Davis LL. Prevalence of post-traumatic stress disorder in the United States: a systematic literature review. Curr Med Res Opin. 2021 Dec;37(12):2151-2161. doi: 10.1080/03007995.2021.1978417. Epub 2021 Sep 23. PMID: 34498953. [↩] [↩]
- Rothbaum BO, Schwartz AC. Exposure therapy for posttraumatic stress disorder. Am J Psychother. 2002;56(1):59-75. doi: 10.1176/appi.psychotherapy.2002.56.1.59. PMID: 11977784. [↩] [↩]
- Tang WK, Wang L, F Tsoi KK, Rutovic S, Kim JS. Post-Traumatic Stress Disorder after Stroke: A Systematic Review. Neurol India. 2022 Sep-Oct;70(5):1887-1895. Doi: 10.4103/0028-3886.359285. PMID: 36352583. [↩] [↩] [↩] [↩]
- Goldfinger JZ, Edmondson D, Kronish IM, Fei K, Balakrishnan R, Tuhrim S, Horowitz CR. Correlates of post-traumatic stress disorder in stroke survivors. J Stroke Cerebrovasc Dis. 2014 May-Jun;23(5):1099-105. doi: 10.1016/j.jstrokecerebrovasdis.2013.09.019. Epub 2013 Oct 19. PMID: 24144593; PMCID: PMC3992186. [↩] [↩]
- Feely D, Slattery B, Walsh T, Galvin T, Donlon K, Hanlon M, Gormley D, Brown GM, Quinn S, Robinson S, Judge C, O’Donnell M, Sarma K, McGuire BE. Acute stress symptoms 1-2 weeks after stroke predict the subsequent development of post-traumatic stress symptoms: A prospective cohort study. PLoS One. 2023 Oct 4;18(10):e0286220. doi: 10.1371/journal.pone.0286220. PMID: 37792802; PMCID: PMC10550116. [↩]
- Meyer EC, La Bash H, DeBeer BB, Kimbrel NA, Gulliver SB, Morissette SB. Psychological inflexibility predicts PTSD symptom severity in war veterans after accounting for established PTSD risk factors and personality. Psychol Trauma. 2019 May;11(4):383-390. doi: 10.1037/tra0000358. Epub 2018 Aug 27. PMID: 30148370. [↩] [↩]
- Kim SH, Lee N, Martin B, Suh J, Walters D, Silverman DH, Berenji GR. Examining posttraumatic stress disorder as a key postinjury risk factor in OIF/OEF veterans with blast-induced mild traumatic brain injury. Neuropsychology. 2020 Sep;34(6):713-725. doi: 10.1037/neu0000678. Epub 2020 Jul 2. PMID: 32614198. [↩] [↩]
- Rutovic S, Kadojic D, Dikanovic M, Solic K, Malojcic B. Prevalence and correlates of post-traumatic stress disorder after ischaemic stroke. Acta Neurol Belg. 2021 Apr;121(2):437-442. doi: 10.1007/s13760-019-01200-9. Epub 2019 Aug 26. PMID: 31452093. [↩] [↩]
- Stein LA, Goldmann E, Zamzam A, Luciano JM, Messé SR, Cucchiara BL, Kasner SE, Mullen MT. Association Between Anxiety, Depression, and Post-traumatic Stress Disorder and Outcomes After Ischemic Stroke. Front Neurol. 2018 Nov 2;9:890. Doi: 10.3389/fneur.2018.00890. PMID: 30450075; PMCID: PMC6224432. [↩] [↩]
- Kiphuth IC, Utz KS, Noble AJ, Köhrmann M, Schenk T. Increased prevalence of posttraumatic stress disorder in patients after transient ischemic attack. Stroke. 2014 Nov;45(11):3360-6. Doi: 10.1161/STROKEAHA.113.004459. Epub 2014 Oct 2. PMID: 25278556. [↩] [↩]
- Edmondson D, Richardson S, Fausett JK, Falzon L, Howard VJ, Kronish IM. Prevalence of PTSD in Survivors of Stroke and Transient Ischemic Attack: A Meta-Analytic Review. PLoS One. 2013 Jun 19;8(6):e66435. Doi: 10.1371/journal.pone.0066435. PMID: 23840467; PMCID: PMC3686746. [↩] [↩]
- Gaffey AE, Rosman L, Burg MM, Haskell SG, Brandt CA, Skanderson M, Dziura J, Sico JJ. Posttraumatic Stress Disorder, Antidepressant Use, and Hemorrhagic Stroke in Young Men and Women: A 13-Year Cohort Study. Stroke. 2021 Jan;52(1):121-129. Doi: 10.1161/STROKEAHA.120.030379. Epub 2020 Dec 10. PMID: 33297868; PMCID: PMC7770089. [↩] [↩] [↩] [↩] [↩] [↩]
- Yu S, Alper HE, Nguyen AM, Maqsood J, Brackbill RM. Stroke hospitalizations, posttraumatic stress disorder, and 9/11-related dust exposure: Results from the World Trade Center Health Registry. Am J Ind Med. 2021 Oct;64(10):827-836. doi: 10.1002/ajim.23271. Epub 2021 Jul 19. PMID: 34558721. [↩] [↩]
- Chen, M. H., Pan, T. L., Li, C. T., Lin, W. C., Chen, Y. S., Lee, Y. C., Tsai, S. J., Hsu, J. W., Huang, K. L., Tsai, C. F., Chang, W. H., Chen, T. J., Su, T. P., & Bai, Y. M. (2015). Risk of stroke among patients with post-traumatic stress disorder: nationwide longitudinal study. The British journal of psychiatry : the journal of mental science, 206(4), 302–307. https://doi.org/10.1192/bjp.bp.113.143610 [↩]
- Perkins JD, Wilkins SS, Kamran S, Shuaib A. Post-traumatic stress disorder and its association with stroke and stroke risk factors: A literature review. Neurobiol Stress. 2021 Apr 25;14:100332. Doi: 10.1016/j.ynstr.2021.100332. PMID: 34026954; PMCID: PMC8122169. [↩]
- Ben Assayag E, Tene O, Korczyn AD, Solomon Z, Bornstein NM, Shenhar-Tsarfaty S, Seyman E, Niry D, Molad J, Hallevi H. Posttraumatic Stress Symptoms After Stroke: The Effects of Anatomy and Coping Style. Stroke. 2022 Jun;53(6):1924-1933. doi: 10.1161/STROKEAHA.121.036635. Epub 2022 Mar 10. PMID: 35264011. [↩] [↩] [↩] [↩] [↩]
- Nisar S, Bhat AA, Hashem S, Syed N, Yadav SK, Uddin S, Fakhro K, Bagga P, Thompson P, Reddy R, Frenneaux MP, Haris M. Genetic and Neuroimaging Approaches to Understanding Post-Traumatic Stress Disorder. Int J Mol Sci. 2020 Jun 4;21(12):4503. doi: 10.3390/ijms21124503. PMID: 32599917; PMCID: PMC7352752.; Ben Assayag E, Tene O, Korczyn AD, Solomon Z, Bornstein NM, Shenhar-Tsarfaty S, Seyman E, Niry D, Molad J, Hallevi H. Posttraumatic Stress Symptoms After Stroke: The Effects of Anatomy and Coping Style. Stroke. 2022 Jun;53(6):1924-1933. doi: 10.1161/STROKEAHA.121.036635. Epub 2022 Mar 10. PMID: 35264011. [↩]
- Tyagi S, Luo N, Tan CS, Tan KB, Tan BY, Menon E, Venketasubramanian N, Loh WC, Fan SH, Yang KLT, Chan ASL, Farwin A, Lukman ZB, Koh GC. Seeking healthcare services post-stroke: a qualitative descriptive study exploring family caregiver and stroke survivor perspectives in an asian setting. BMC Neurol. 2021 Nov 5;21(1):429. doi: 10.1186/s12883-021-02463-7. PMID: 34740323; PMCID: PMC8569985. [↩] [↩]
- Deutschbein J, Grittner U, Schneider A, Schenk L. Community care coordination for stroke survivors: results of a complex intervention study. BMC Health Serv Res. 2020 Dec 19;20(1):1143. Doi: 10.1186/s12913-020-05993-x. PMID: 33341112; PMCID: PMC7749985. [↩] [↩]
- Jiang C, Li Z, Wang J, Liu L, Luo G, Zheng X. Effectiveness of repetitive transcranial magnetic stimulation combined with a brief exposure procedure for post-stroke posttraumatic stress disorder. J Affect Disord. 2023 Apr 1;326:89-95. doi: 10.1016/j.jad.2023.01.096. Epub 2023 Jan 28. PMID: 36717030. [↩] [↩] [↩]
- Ducasse D, Fond G. La thérapie d’acceptation et d’engagement [Acceptance and commitment therapy]. Encephale. 2015 Feb;41(1):1-9. French. doi: 10.1016/j.encep.2013.04.017. Epub 2013 Nov 18. PMID: 24262333. [↩] [↩] [↩] [↩]
- Hsu T, Adamowicz JL, Thomas EBK. The effect of acceptance and commitment therapy on the psychological flexibility and inflexibility of undergraduate students: A systematic review and three-level meta-analysis. J Contextual Behav Sci. 2023 Oct;30:169-180. Doi: 10.1016/j.jcbs.2023.10.006. Epub 2023 Oct 26. PMID: 37982074; PMCID: PMC10655902. [↩] [↩]
- Jiang C, Li Z, Du C, Zhang X, Chen Z, Luo G, Wu X, Wang J, Cai Y, Zhao G, Bai H. Supportive psychological therapy can effectively treat post-stroke post-traumatic stress disorder at the early stage. Front Neurosci. 2022 Oct 6;16:1007571. Doi: 10.3389/fnins.2022.1007571. PMID: 36278005; PMCID: PMC9583431.; Tyagi S, Luo N, Tan CS, Tan KB, Tan BY, Menon E, Venketasubramanian N, Loh WC, Fan SH, Yang KLT, Chan ASL, Farwin A, Lukman ZB, Koh GC. Seeking healthcare services post-stroke: a qualitative descriptive study exploring family caregiver and stroke survivor perspectives in an asian setting. BMC Neurol. 2021 Nov 5;21(1):429. doi: 10.1186/s12883-021-02463-7. PMID: 34740323; PMCID: PMC8569985. [↩]
- Chang RS, Leung WC, Vassallo M, Sykes L, Battersby Wood E, Kwan J. Antiepileptic drugs for the primary and secondary prevention of seizures after stroke. Cochrane Database Syst Rev. 2022 Feb 7;2(2):CD005398. doi: 10.1002/14651858.CD005398.pub4. PMID: 35129214; PMCID: PMC8819727. [↩]
- Tang WK, Wang L, F Tsoi KK, Rutovic S, Kim JS. Post-Traumatic Stress Disorder after Stroke: A Systematic Review. Neurol India. 2022 Sep-Oct;70(5):1887-1895. Doi: 10.4103/0028-3886.359285. PMID: 36352583.; Chen, M. H., Pan, T. L., Li, C. T., Lin, W. C., Chen, Y. S., Lee, Y. C., Tsai, S. J., Hsu, J. W., Huang, K. L., Tsai, C. F., Chang, W. H., Chen, T. J., Su, T. P., & Bai, Y. M. (2015). Risk of stroke among patients with post-traumatic stress disorder: nationwide longitudinal study. The British journal of psychiatry : the journal of mental science, 206(4), 302–307. https://doi.org/10.1192/bjp.bp.113.143610 [↩]
- van Tuijl JH, van Raak EPM, van Oostenbrugge RJ, Aldenkamp AP, Rouhl RPW. Treatment with Diazepam in Acute Stroke Prevents Poststroke Seizures: A Substudy of the EGASIS Trial. Cerebrovasc Dis. 2021;50(2):216-221. doi: 10.1159/000512799. Epub 2021 Jan 19. PMID: 33465768.; El Husseini N, Katzan IL, Rost NS, Blake ML, Byun E, Pendlebury ST, Aparicio HJ, Marquine MJ, Gottesman RF, Smith EE; American Heart Association Stroke Council; Council on Cardiovascular and Stroke Nursing; Council on Cardiovascular Radiology and Intervention; Council on Hypertension; and Council on Lifestyle and Cardiometabolic Health. Cognitive Impairment After Ischemic and Hemorrhagic Stroke: A Scientific Statement From the American Heart Association/American Stroke Association. Stroke. 2023 Jun;54(6):e272-e291. doi: 10.1161/STR.0000000000000430. ; Jiang C, Li Z, Du C, Zhang X, Chen Z, Luo G, Wu X, Wang J, Cai Y, Zhao G, Bai H. Supportive psychological therapy can effectively treat post-stroke post-traumatic stress disorder at the early stage. Front Neurosci. 2022 Oct 6;16:1007571. Doi: 10.3389/fnins.2022.1007571. PMID: 36278005; PMCID: PMC9583431. [↩]
- Gaffey AE, Rosman L, Burg MM, Haskell SG, Brandt CA, Skanderson M, Dziura J, Sico JJ. Posttraumatic Stress Disorder, Antidepressant Use, and Hemorrhagic Stroke in Young Men and Women: A 13-Year Cohort Study. Stroke. 2021 Jan;52(1):121-129. Doi: 10.1161/STROKEAHA.120.030379. Epub 2020 Dec 10. PMID: 33297868; PMCID: PMC7770089.; Jiang C, Li Z, Du C, Zhang X, Chen Z, Luo G, Wu X, Wang J, Cai Y, Zhao G, Bai H. Supportive psychological therapy can effectively treat post-stroke post-traumatic stress disorder at the early stage. Front Neurosci. 2022 Oct 6;16:1007571. Doi: 10.3389/fnins.2022.1007571. PMID: 36278005; PMCID: PMC9583431.; Tyagi S, Luo N, Tan CS, Tan KB, Tan BY, Menon E, Venketasubramanian N, Loh WC, Fan SH, Yang KLT, Chan ASL, Farwin A, Lukman ZB, Koh GC. Seeking healthcare services post-stroke: a qualitative descriptive study exploring family caregiver and stroke survivor perspectives in an asian setting. BMC Neurol. 2021 Nov 5;21(1):429. doi: 10.1186/s12883-021-02463-7. PMID: 34740323; PMCID: PMC8569985. [↩]
- Jiang C, Li Z, Wang J, Liu L, Luo G, Zheng X. Effectiveness of repetitive transcranial magnetic stimulation combined with a brief exposure procedure for post-stroke posttraumatic stress disorder. J Affect Disord. 2023 Apr 1;326:89-95. doi: 10.1016/j.jad.2023.01.096. Epub 2023 Jan 28. PMID: 36717030.; Jiang C, Li Z, Du C, Zhang X, Chen Z, Luo G, Wu X, Wang J, Cai Y, Zhao G, Bai H. Supportive psychological therapy can effectively treat post-stroke post-traumatic stress disorder at the early stage. Front Neurosci. 2022 Oct 6;16:1007571. Doi: 10.3389/fnins.2022.1007571. PMID: 36278005; PMCID: PMC9583431. [↩] [↩]
- Clinic, C. (2024, July 22). What happens during fight-or-flight response?. Cleveland Clinic. https://health.clevelandclinic.org/what-happens-to-your-body-during-the-fight-or-flight-r sponse [↩]
- Doria JW, Forgacs PB. Incidence, Implications, and Management of Seizures Following Ischemic and Hemorrhagic Stroke. Curr Neurol Neurosci Rep. 2019 May 27;19(7):37. doi: 10.1007/s11910-019-0957-4. PMID: 31134438; PMCID: PMC6746168. [↩]
- Feely D, Slattery B, Walsh T, Galvin T, Donlon K, Hanlon M, Gormley D, Brown GM, Quinn S, Robinson S, Judge C, O’Donnell M, Sarma K, McGuire BE. Acute stress symptoms 1-2 weeks after stroke predict the subsequent development of post-traumatic stress symptoms: A prospective cohort study. PLoS One. 2023 Oct 4;18(10):e0286220. doi: 10.1371/journal.pone.0286220. PMID: 37792802; PMCID: PMC10550116. [↩]
- Foundation, S. awareness. (2023, July 11). Stroke facts & statistics. Stroke Awareness Foundation. https://www.strokeinfo.org/stroke-facts-statistics/#:~:text=Someone%20has%20a%20str ke%20every,disability%20in%20the%20United%20States. [↩]
- Hansen M, Ross J, Armour C. Evidence of the dissociative PTSD subtype: A systematic literature review of latent class and profile analytic studies of PTSD. J Affect Disord. 2017 Apr 15;213:59-69. Doi: 10.1016/j.jad.2017.02.004. Epub 2017 Feb 7. PMID: 28192736. [↩]
- Schneck M, & Orjuela K, & Rubinos C (2016). Stroke neurology. Salardini A, & Biller J(Eds.), The HospitalNeurology Book. McGraw-Hill Education. https://neurology.mhmedical.com/content.aspx?bookid=1779§ionid=122853486 [↩]
- Wolf EJ, Hawn SE, Sullivan DR, Miller MW, Sanborn V, Brown E, Neale Z, Fein- Schaffer D, Zhao X, Logue MW, Fortier CB, McGlinchey RE, Milberg WP. Neurobiological and genetic correlates of the dissociative subtype of posttraumatic stress disorder. J Psychopathol Clin Sci. 2023 May;132(4):409-427. doi: 10.1037/abn0000795. Epub 2023 Apr 6. PMID: 37023279; PMCID: PMC10286858. [↩]






