Abstract
This study determines the impact of collectivist attitudes in vaccine hesitancy of East Asians in Canada and the U.S. that frequently display lower vaccination rates than other populations. Previous literatures focused on the impact of cultural dimensions in health behaviors, but detailed analysis of the impact of those on specific ethnicities in multi-ethnic nations are lacking. The study used a 2022 survey on COVID-19 quarantine policies in Canada and the U.S. (N = 2736). Three Poisson models, two with and without collectivist variables, measured by attachment anxiety, and one taking account of its interaction with ethnicity, predicted vaccine hesitancy with common confounders of risk perception and vaccination attitude. While East Asians were more hesitant to receive vaccination when adjusting for common confounders, those with higher collectivist attitudes were more likely to get vaccinated considering the entire population. Models taking account of collectivist variables displayed lower Akaike Information Criterion scores and lower chi-square deviances. The model taking account of the interaction displayed that collectivism played a more significant role among East Asians, which higher levels of collectivism were associated with increase in vaccine hesitancy, a trend that deviates from previous literatures conducted with datasets constructed in their countries of origin. Mediators were identified and tested for internal consistency and statistical significance. While no significant degree of mediation was identified, moderate Cronbach Alpha values and low pairwise Pearson’s correlation coefficients suggested some level of multidimensionality. Findings can be utilized in vaccination policies or campaigns when targeting East Asians in multi-ethnic countries.
Introduction
COVID-19, a respiratory disease that was first confirmed in Wuhan on December 12, 2019, brought significant changes not only to global health, but also to disease prevention strategies and government policies regarding disease control in many countries. From its first outbreak to July 6, 2024, the pandemic prompted more than 776 million reported cases and 7.1 million reported deaths worldwide1. The United States under the Trump administration primarily focused on establishing local drive-through testing sites while rapidly deploying vaccines to the public through Operation Warp Speed (OWS)2. In contrast, South Korea focused on tracking potential disease carriers through GPS tracking, credit card usage records, and other personal information3. Despite multiple tactics, vaccination has been the most effective method for COVID-19 disease control4. However, many individuals worldwide are hesitant to receive vaccination, often referred as vaccine hesitancy. One observed trend is that East Asian nations like South Korea and Japan consistently demonstrate higher vaccination rates than Western countries such as the United States and Canada. Both South Korea and Japan initiated vaccination since February 2021, and reached vaccination rates of 70% and 60% respectively by mid-2021 while the United States and Canada demonstrated similar vaccination rates despite deploying vaccines much earlier5’6’7’8. A significant difference between East Asian countries and Western countries are cultural norms, particularly collectivism. According to Hofstede’s Cultural Dimensions Theory, South Korea scores 18 on the individualism index, an index developed to measure the degree of individualistic characteristic of nations, demonstrating the lowest level of individualistic characteristics out of the 31 sampled countries, while the U.S. scores 91, the highest9. Prior research concludes that collectivism has a positive relationship with vaccination intent in East Asians in their countries of origin, but some East Asian populations within multi-ethnic western countries like the U.S. and Canada display lower vaccination rates than other populations despite their cultural norms10. The research hypothesized that collectivist attitude in East Asian minorities is associated with higher vaccine hesitancy compared to other ethnicities unlike its role in East Asian nations.
Methodology
1. Dataset
A web-based survey targeting adults residing in the four most populous states in the United States of America: New York, California, Florida, and Texas and English-speaking regions of Canada was utilized for statistical analysis11. The survey asks individuals for socio-demographic characteristics, vaccination status, vaccination intent, and opinions on current COVID-19 quarantine policies. 2736 participants who fully completed the survey during survey wave 3, the most recent wave, in March of 2021 were selected for analysis.
2. Measures
Vaccine hesitancy was selected as the dependent variable, ranging discretely from 1 to 6, which 6 represented the highest vaccine hesitancy and 1 represented the lowest. The item asking the degree of vaccine acceptance was reverse coded to represent vaccine hesitancy. Collectivism in this study is characterized as the concern by a person about the effects of actions or decisions on others12.
Collectivist attitude was measured by attachment anxiety computed based on the Experiences in Close Relationships (ECR) scale. The Garretson survey utilized the ECR-M16 model13. Attachment anxiety was represented by the mean of the responses in the items with even numberings, which higher scores represented higher attachment anxiety, and collectivist traits. The ECR-M16 Attachment Anxiety Scale was utilized as a proxy measure for collectivism because the dataset did not contain explicit scales to measure collectivism directly. This was to avoid errors and misrepresentations by measuring collectivist attitude based on an item or a combination of those not intended by Garretson. Aghishtein et al. (2013) assessed the relationship between collectivism and attachment anxiety in a sample of multicultural college students. Collectivism was measured by a scale adapted from general collectivistic traits presented by Hofstede’s cultural dimensions theory and attachment anxiety was measured by the ECR-R scale. Attachment anxiety was strongly correlated with high levels with collectivism, and regardless of country of origin, individuals with stronger collectivist traits demonstrated higher attachment anxiety14. Frias et al. (2014) utilized a sample of people from the U.S. and Mexico and discovered that attachment Anxiety was a statistically significant predictor of collectivism and showed positive association15.
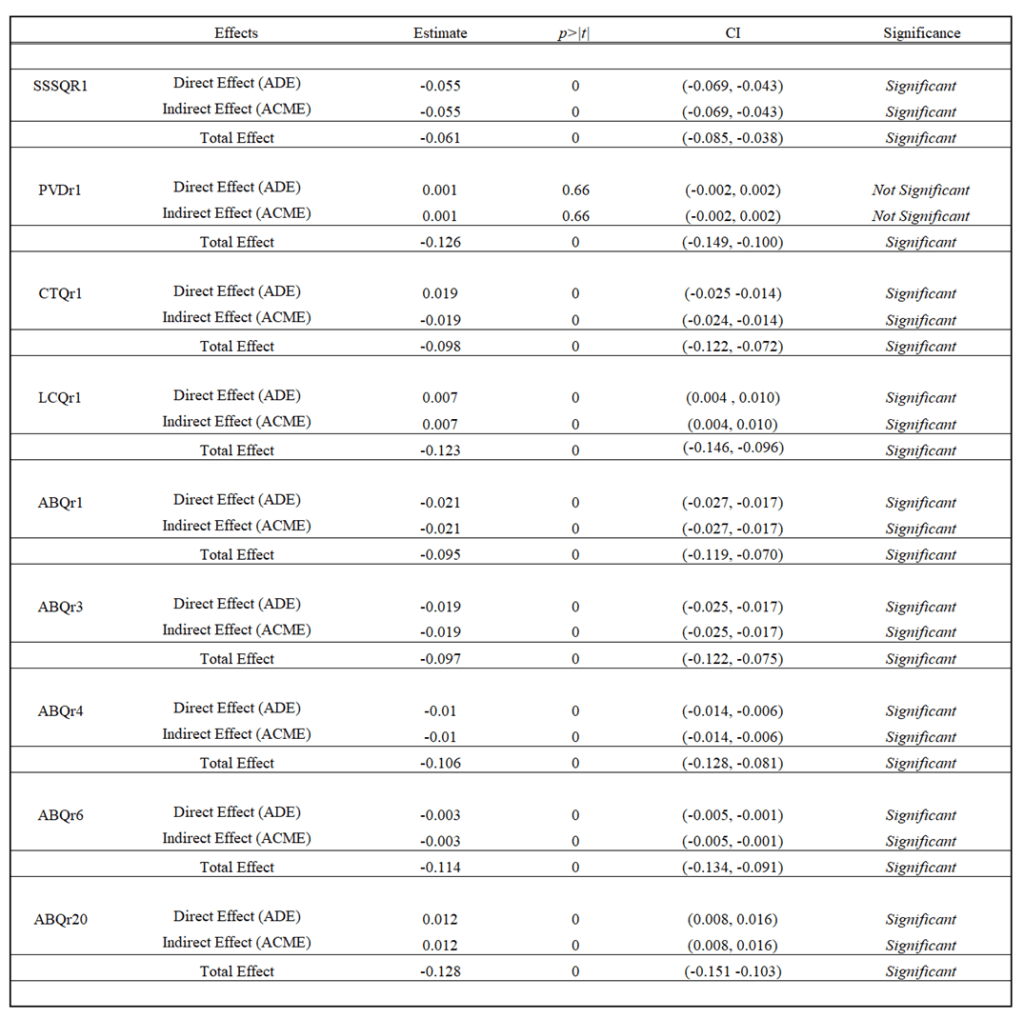
Potential significant mediators relating to both attachment anxiety and collectivism were selected with statistical rigor in the context of epidemiology16. All variables identified as potential mediators were evaluated to somewhat measure the degree of collectivism in respondents. SSSQr1 is the set of collected responses with the prompt “I am easily influenced by other people’s opinions” with a Likert scale from 1 to 5, 1 being “Not at all” and 5 being “A lot”; PVDr1 is the set of collected responses with the prompt “It really bothers me when people sneeze without covering their mouths” with a Likert Scale of 1 to 7, 1 being “Strongly disagree” and 7 being “Strongly agree”; CTQr1 is the set of collected responses with the prompt “When it concerns COVID-19, all levels of government are capable” with a scale of 1 to 5, 1 being “Strongly disagree” and 5 being “Strongly agree”; LCQr1 is the set of collected responses with the prompt “My life is determined by my own actions” with a scale of 1 to 7, 1 being “Strongly disagree and 7 being “Strongly agree”. Variables ABQr1, ABQr3, ABQr4, ABQr6, and ABQr20 utilized identical Likert Scales with a scale of 1 to 5, 1 being “Strongly disagree” and 5 being “Strongly agree”. ABQr1 is the set of collected responses with the prompt “Do you listen attentively to what older people say about how you should behave?”; ABQr3 is the set of collected responses with the prompt “When a person in authority whom you trust tells you to do something, do you do it, even though you can’t see the reason for it?”; ABQr4 is the set of collected responses with the prompt “Do you criticize people who are rude to their superiors?”; ABQr6 is the set of collected responses with the prompt “When you go to work, do you dress so as to be acceptable to the people who run the place?”; ABQr20 is the set of collected responses with the prompt “Do you stand when they play the National Anthem in public?”.
3. Statistical Analysis
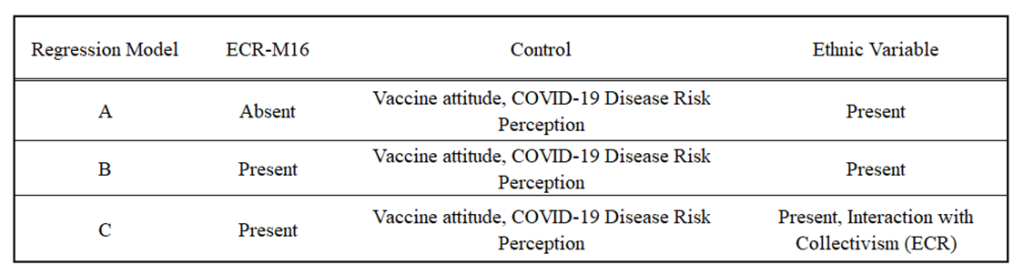
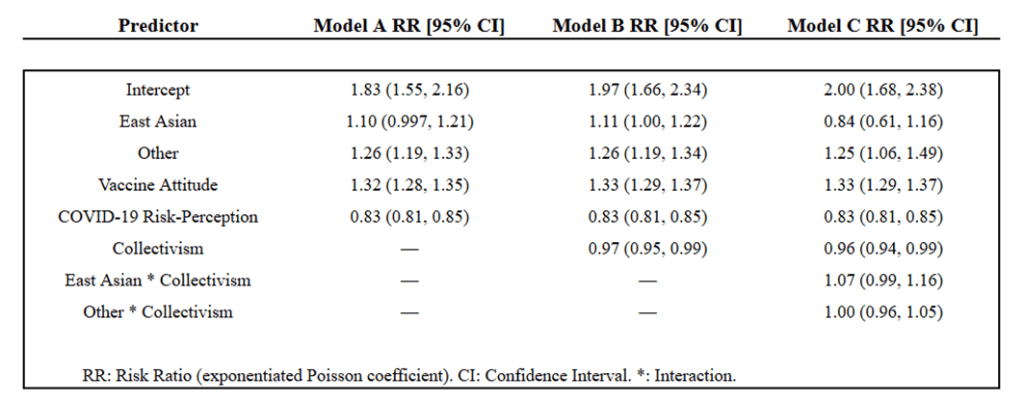
Poisson regression assessed the association of ethnicity and collectivistic attitude variables to vaccination hesitancy adjusting for common confounders of vaccine attitude and COVID-19 disease risk perception. A log-likelihood ratio test was conducted between the negative binomial model and the Poisson model. The Pearson Chi-Squared Dispersion Statistic was 1, indicating that no overdispersion was present. Also, and λ (lambda, mean) of the Poisson distribution was constant, indicating that the Poisson model was appropriate for the analysis of the context17.Races were divided in to White, East Asian, and Other, and the White respondents were used as the reference group. Models were run with and without collectivist variables, ECR-M16, and a separate model taking account of interaction between ethnicity and collectivist variables were also tested (Table 1). The fit of the three models were compared with the Akaike Information Criterion (AIC) test. All explanatory variables were normalized.
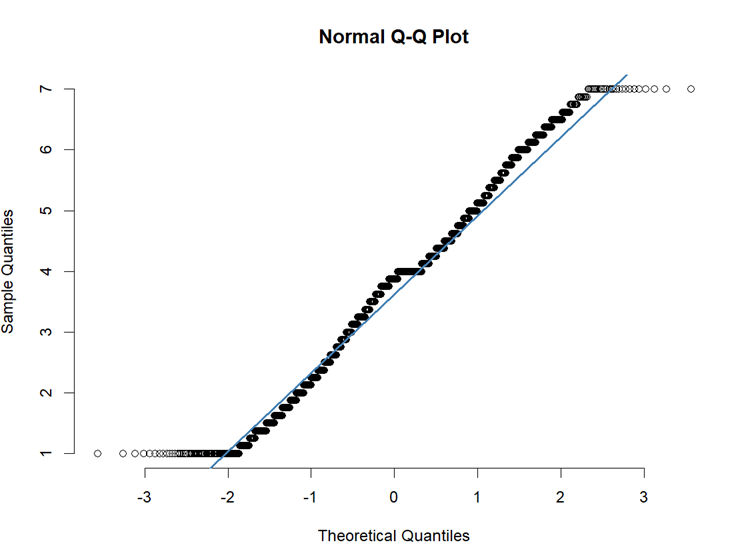
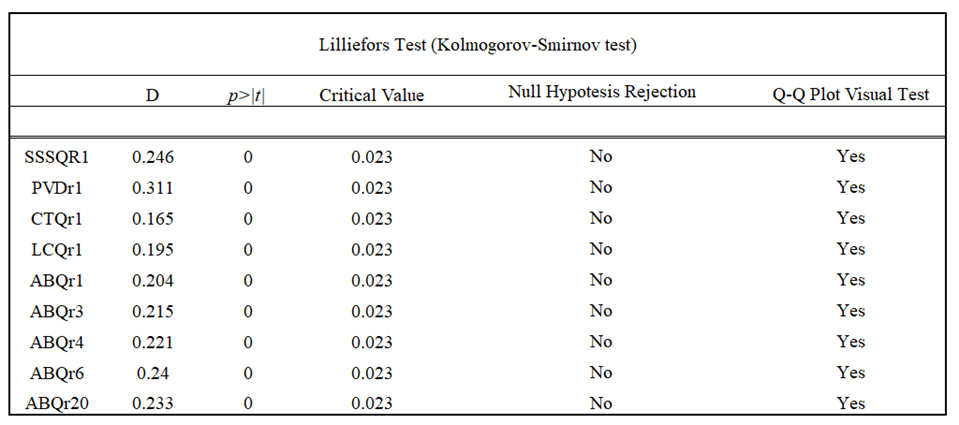
Internal consistency of the set of potential mediators were assessed with the Cronbach Alpha value, which were deployed even though the Lilliefors test for normality rejected the hypothesis for normal distribution (p < 2.2e-16). Due to conditional insignificance of normality tests in large number of samples,the distribution of variables assessing for collectivism was determined to be pertinent to assess their internal consistencies via Cronbach Alpha by visual inspection of the Quantile-Quantile plots (Figure 1, Table 2)18.
The set of potential mediators displayed a Cronbach Alpha value of 0.62, displaying acceptable internal consistency for further mediator analysis19, supported by thresholds in previous literature. The development of Health Behavior Motivation Scale by Poraj-Weder et al. (2021) involved the assessment of internal consistencies of its subscales, which ranging from 0.62 to 0.82, which the researchers determined acceptable for the exploratory stage of the research20. Hu et al. (2024) explored the impact of chronic diseases in quality of life of middle-aged men. They utilized the dataset from the China Health and Retirement Longitudinal Study (CHARLS), which included a 5-questionaire set to measure degree of digitization of men of chronic illness. Researchers used the Alpha value of 0.60 as the minimum threshold when evaluating if the item set was reliable for measuring digitization21.
A correlation matrix assessing multicollinearity among those variables was deployed, but no significant correlation (r > 0.3) was detected in context of the research field, suggesting some degree of multidimensionality amongst them (Figure 2)22. Selected Mediators were tested for Average Casual Mediation Effect (ACME), Average Marginal Effect (AME), and Total Effect using the formula which took account of ethnicity and collectivism, but not their interaction (Model B). Mediation effect was considered statistically significant if 95% confidence intervals for each effect excluded 0 and p < 0.05.
All statistical analysis were done with R (version 4.3.3) and packages dplyr (version 1.1.4), tidyverse (version 4.3.3), foreign (version 0.8-87), corrplot (version 0.94), and psych (version 2.4.12)23’24’25’26’27
Results
1. Descriptive Results (Table 3)
52% of East Asians were willing to definitely receive vaccination, higher than respondents of other ethnicities yet lower than the white respondents. Vaccine attitudes varied by ethnicity, White being the least hesitant and other ethnicities being the most. Experiences in close relationships did not vary significantly across ethnicities.
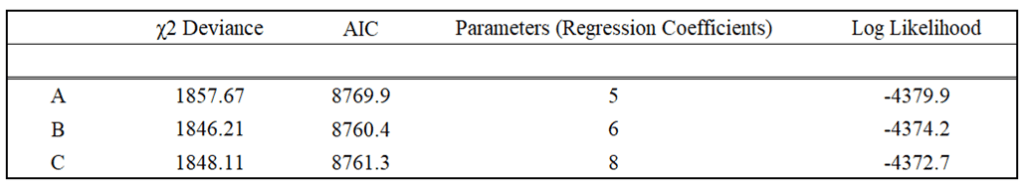
2. Model Analysis (Table 4)
Models with attachment (models A and B) have lower AIC than without, suggesting that adjusting for close relationships better estimates vaccine hesitancy. Likelihood ratio tests were conducted between models A and B and models B and C. The decrease in chi-square deviance of 11.46 from model A to B suggests that inclusion of ECR in models significant improved model fit. Collectivism contributed meaningfully to explaining vaccine hesitancy. The chi-square deviance decrease of 3.10 from model B to C indicated that adding the interaction term did not significantly improve model fit in comparison to the addition of parameters. Predicting vaccine hesitancy of all respondents, models A and B displayed AICs of 8769.9, 8760.4, respectively, and the model C displayed AIC of 8761.3. Test for interaction showed no significant difference on the degree of impact of collectivism on vaccine hesitancy between ethnicities but a trend of greater influence on vaccine hesitancy for East Asians.
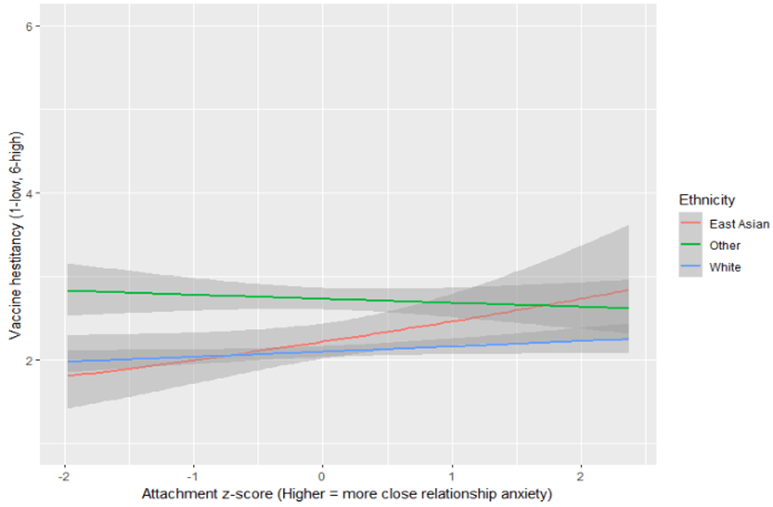
3. Regression Analysis (Table 5, Figure 6)
East Asians were 10% less likely to get vaccinated in comparison to White population, but more likely than other minorities when adjusting for COVID-19 risk perception and vaccination attitudes. East Asians were 11% less likely to get vaccinated when collectivism was introduced as a variable. When the interaction of ethnicity and collectivism was taken account, East Asians were 16% more likely to receive vaccination than White respondents. Respondents of other ethnicities were 25% to 26% more hesitant to receive vaccination than White respondents across all 3 models controlling for COVID-19 risk perception and vaccine attitudes. Model B indicates increase in ECR Attention Anxiety scale by 1 typically resulted in 3% to 4% decrease in vaccine hesitancy. Among East Asians, each point increase in collectivism was associated with a 7% weaker protective effect than among White respondents while the effect of interaction between collectivism and ethnicities were same for both respondents of White and Other ethnicities.
4. Mediation Analysis (Table 6)
The total effect of all mediators was statistically significant, but test for mediation displayed no significant magnitude of mediation through selected variables (Table 3).
Discussion
This study examined the relationship between collectivist attitudes and COVID-19 vaccine hesitancy among East Asian minorities, focusing on how collectivism impacted East Asians in North America compared to other ethnicities. The study contributes to the gap in existing literature, where the focus on impact of cultural traits like collectivism on vaccine uptake of specific ethnicities living outside their countries of origins are peripheral. The research addresses the difference in vaccine hesitancy among some East Asians despite prevalence of collectivist traits in both their countries of origin and North America.
Higher degree of collectivist traits increased vaccine hesitancy among East Asians yet when the interaction of ethnicity and collectivism was taken account, East Asians were significantly more likely to get vaccinated. At an average level of collectivist traits in respect to East Asians, they were significantly more likely to get vaccinated than both White respondents and those of other ethnicities. However, higher collectivist traits reversed the role shown in their countries of origin, negatively impacting vaccine uptake chances.
One possible explanation may be the difference in institutional trust between East Asians in North America and in their countries of origin. In Asian countries, collectivism aligns with trust in institutions28. Based on two waves of the European Social Survey and multiple regional datasets of European nations, Kaasa and Andriani concluded that higher levels of individualism are correlated with lower social and institutional trust29. However, despite high levels of collectivism compared to other ethnicities, East Asian minorities may not exhibit same level of institutional trust in host countries. Mistrust in institutions like government and public medical support are predictors of vaccine hesitancy. This may be because other factors than collectivism such as general institutional mistrust in diaspora communities and political orientations.
Also, different social norms and characteristics, particularly individualist culture of North America compared to collectivist culture of East Asian countries, may pose significant stress to East Asian Minorities in North America. Mera-Lemp et al. presented that Latin American immigrants in Chile experience significant degree of acculturated stress due to difference in social norms regarding individualism and collectivism30. Khongyot et al. demonstrates that undergraduate students in healthcare related studies displayed higher vaccine hesitancy when they had high stress levels31. East Asian minorities with acculturated stress, which those more collectivist would experience more significantly, may display higher vaccine hesitancy compared to other ethnicities.
Public Health campaigns and advertisements that appeal to collectivist values such as mentioning one’s close communities may not be effective and even detrimental in vaccine uptake to some ethnic groups like East Asian minorities in North America. The research revealed that collectivism, a shared trait between East Asians in North America and their countries of origin, demonstrate different effects on vaccine uptake. This implies that approach to vaccination must be evaluated considering the target populations’ ethical background.
Results regarding ethnic collectivistic attitudes and social relationships align with the study from Konstantinou et al. which explores vaccination uptake based on Social Contagion Theory32 This study focused in East Asians in multi-ethnic countries regarding COVID-19 vaccination.
Vaccine hesitancy and vaccination rates vary much by states and provinces. Variables which depend on geographical regions such as annual household income, education level, degree of public health infrastructure, and political orientations can confound with the effects of collectivism on vaccine hesitancy. This research did not account for fixed effects as number of respondents were too few for some regions. Regarding those regions, it was considered inappropriate to assume the dataset itself captured meaningful regional differences. Due to limitations in computing power, the number of bootstrapping for mediation analysis were less than 5000 iterations, an adequate number for the size of the dataset. Also, despite the visual inspections of the Q-Q plots of mediators, some of them might not have been normally distributed to a pertinent extent for deploying Cronbach Alpha to measure their internal consistency and thereby could have lowered the credibility of the values. Moderate degree of internal consistency among questionnaire of selected mediators yet low pairwise correlation coefficients amongst them suggests some degree of multidimensionality, impacting the reliability of computed mediation impact. Causal relationships cannot be made between predictors, mediators, and outcome variables because there was no temporal separation between the three; the survey measured them at one timepoint. Future studies could explore longitudinal effects, as collectivist values may change over time with exposure to individualistic societies.
Conclusion
While East Asians residing in the U.S. and Canada exhibited greater vaccine hesitancy compared to White and other ethnicities adjusting for disease seriousness and vaccine effectiveness and interaction between collectivism and ethnicity played the biggest role among the three groups. (RR 1.07 vs 1.00) Collectivism was associated with increase in vaccine hesitancy considering only East Asians, but considering the entire population, those with higher sense of collectivism were less hesitant to receive vaccination. Results may be applied in vaccination advertisement creation in future outbreaks targeting East Asians in North America.
References
- World Health Organization. “COVID-19 Deaths Dashboard.” World Health Organization, 2023, https://data.who.int/dashboards/covid19/deaths. Accessed 8 Feb. 2025. [↩]
- U.S. Government Accountability Office. Operation Warp Speed: Accelerated COVID-19 Vaccine Development Status and Efforts to Address Manufacturing Challenges. GAO-21-319, 11 Feb. 2021, www.gao.gov/products/gao-21-319. Accessed 8 Feb. 2025. [↩]
- Chloe Jeongjin Lee, Yeonsu Kim, Gangju Lee, Kiryong Nam, Benimana Dieudonne Theos, Seungpil Jung, Woojoo Lee, Juhwan Oh, Seung-sik Hwang, Dasol Kim. Comparative Analysis of International Coronavirus Disease 2019 Contact-Tracing, Isolation, and Quarantine (TIQ) Policies and Simulation of Policy Effects. Public Health Weekly Report 2024;17:1267-1284. https://doi.org/10.56786/PHWR.2024.17.30.1 [↩]
- World Health Organization. “COVID-19 Vaccines: WHO Advice.” World Health Organization, 2023, https://www.who.int/emergencies/diseases/novel-coronavirus-2019/covid-19-vaccines/advice. Accessed 8 Feb. 2025. [↩]
- Korean Disease Control and Prevention Agency. “2021년 코로나19 예방접종 이렇게 진행됐습니다.” Korean Disease Control and Prevention Agency, 31 Dec. 2021, https://www.kdca.go.kr/gallery.es?mid=a20503010000&bid=0002&list_no=145484&act=view. Accessed 8 Feb. 2025. [↩]
- Ministry of Foreign Affairs of Japan. Japan’s Foreign Policy in a Changing World. Ministry of Foreign Affairs of Japan, 2020, https://www.mofa.go.jp/files/100536486.pdf. Accessed 8 Feb. 2025. [↩]
- Centers for Disease Control and Prevention. COVID-19 Vaccinations in the United States – County. Centers for Disease Control and Prevention, 2023, https://data.cdc.gov/Vaccinations/COVID-19-Vaccinations-in-the-United-States-County/8xkx-amqh/about_data. Accessed 8 Feb. 2025. [↩]
- Public Health Agency of Canada. COVID-19 Vaccination Coverage in Canada. Public Health Agency of Canada, 2023, https://health-infobase.canada.ca/covid-19/vaccination-coverage/. Accessed 8 Feb. 2025. [↩]
- Yoo, JS. & Lee, YJ. National Culture and Tax Avoidance of Multinational Corporations. Sustainability. https://doi.org/10.3390/su11246946 (2009). [↩]
- Cheng, S. K. Understanding the Culture and Behaviour of East Asians–A Confucian Perspective. Australian & New Zealand Journal of Psychiatry, vol. 24, no. 4, 1990, pp. 510–515. https://doi.org/10.3109/00048679009062907. [↩]
- Gerretsen, P., Kim, J., Caravaggio, F., Quilty, L., Sanches, M., Wells, S., Brown, E. E., Agic, B., Pollock, B. G., & Graff-Guerrero, A. (2021). Individual determinants of COVID-19 vaccine hesitancy. PLOS ONE, 16(11), e0258462. https://doi.org/10.1371/journal.pone.0258462 [↩]
- Hui, C. H., & Triandis, H. C. (1986). Individualism-Collectivism: A Study of Cross-Cultural Researchers. Journal of Cross-Cultural Psychology, 17(2), 225-248. https://doi.org/10.1177/0022002186017002006 (Original work published 1986) [↩]
- Philipp, Rebecca, et al. “Attachment Insecurity in Advanced Cancer Patients: Psychometric Properties of the German Version of the Brief Experiences in Close Relationships Scale (ECR-M16-G).” Journal of Pain and Symptom Management, vol. 54, no. 4, Oct. 2017, pp. 555–562, https://doi.org/10.1016/j.jpainsymman.2017.07.026. Accessed 28 Apr. 2021. [↩]
- Agishtein, Peryl & Brumbaugh, Claudia. (2013). Cultural variation in adult attachment: The impact of ethnicity, collectivism, and country of origin. Journal of Social, Evolutionary, and Cultural Psychology. 7. 384. 10.1037/h0099181. [↩]
- Fr´ıas, M.T., Shaver, P.R., & D´ıaz-Loving, R. (2014). Individualism and collectivism as moderators of the association between attachment insecurities, coping, and social support. Journal of Social and Personal Relationships, 31, 3–31. doi:10.1177/0265407513484631 [↩]
- Pallant, Julie. “A Guide to Appropriate Use of Correlation Coefficient in Medical Research.” PubMed Central, 2013, https://pmc.ncbi.nlm.nih.gov/articles/PMC3576830/. Accessed 8 Feb. 2025. [↩]
- “McCullagh, P. And Nelder, J.A. (1989) Generalized Linear Models. 2nd Edition, Chapman and Hall, London. – References – Scientific Research Publishing.” Scirp.org, 2016, scirp.org/reference/referencespapers?referenceid=1851775. Accessed 7 Nov. 2024. [↩]
- Ford, Clay. Understanding QQ Plots. University of Virginia Library, 26 Aug. 2015, https://library.virginia.edu/data/articles/understanding-q-q-plots. Accessed 8 Feb. 2025. [↩]
- Psychometric evaluation of the perceived access to health care questionnaire – Scientific Figure on ResearchGate. Available from: https://www.researchgate.net/figure/The-Cronbachs-alpha-coefficient-for-the-Perception-of-Access-to-Health-care-services_tbl2_352932738 [accessed 8 Feb 2025] [↩]
- Poraj-Weder M, Pasternak A, Szulawski M. The Development and Validation of the Health Behavior Motivation Scale. Front Psychol. 2021 Sep 3;12:706495. doi: 10.3389/fpsyg.2021.706495. PMID: 34539508; PMCID: PMC8446656. [↩]
- Hu, Y., Yang, Y., Gao, Y. et al. The impact of chronic diseases on the health-related quality of life of middle-aged and older adults: the role of physical activity and degree of digitization. BMC Public Health 24, 2335 (2024). https://doi.org/10.1186/s12889-024-19833-8 [↩]
- Dunn, Timothy D., et al. “Evaluating the Differences Between Cronbach’s Alpha and McDonald’s Omega: A Multidimensional Approach.” Journal of Research in Personality, vol. 51, 2014, pp. 27-38. ScienceDirect, https://doi.org/10.1016/j.jrp.2014.05.004. Accessed 8 Feb. 2025. [↩]
- R Core Team (2024). _R: A Language and Environment for Statistical Computing_. R Foundation for Statistical Computing, Vienna, Austria. <https://www.R-project.org/>. [↩]
- Wickham H, François R, Henry L, Müller K, Vaughan D (2023). _dplyr: A Grammar of Data Manipulation_. R package version 1.1.4, <https://CRAN.R-project.org/package=dplyr>. [↩]
- Wickham H, Averick M, Bryan J, Chang W, McGowan LD, François R, Grolemund G, Hayes A, Henry L, Hester J, Kuhn M, Pedersen TL, Miller E, Bache SM, Müller K, Ooms J, Robinson D, Seidel DP, Spinu V, Takahashi K, Vaughan D, Wilke C, Woo K, Yutani H (2019). “Welcome to the tidyverse.” Journal of Open Source Software_, *4*(43), 1686. doi:10.21105/joss.01686 <https://doi.org/10.21105/joss.01686>. [↩]
- R Core Team (2024). _foreign: Read Data Stored by ‘Minitab’, ‘S’, ‘SAS’, ‘SPSS’, ‘Stata’, ‘Systat’, ‘Weka’, ‘dBase’, …_. R package version 0.8-87, <https://CRAN.R-project.org/package=foreign>. [↩]
- Taiyun Wei and Viliam Simko (2024). R package ‘corrplot’: Visualization of a Correlation Matrix (Version 0.94). Available from https://github.com/taiyun/corrplot, William Revelle (2024). _psych: Procedures for Psychological, Psychometric, and Personality Research_. Northwestern University, Evanston, Illinois. R package version 2.4.12, <https://CRAN.R-project.org/package=psych>. [↩]
- Yang, Qing. (2013). A political story of political trust: Institutional settings, political performance, and political trust in East Asia. [↩]
- Kaasa, Anneli & Andriani, Luca. (2021). Determinants of institutional trust: the role of cultural context. Journal of Institutional Economics. 18. 1-21. 10.1017/S1744137421000199. [↩]
- Acculturation orientations, acculturative stress and psychological well-being on Latin American immigrants settled in Santiago, Chile Acta Colombiana de Psicología, vol. 23, no. 1, pp. 231-244, 2020Universidad Catolica de Colombia [↩]
- Khongyot, T., Takyi, A., Ndzeshang, D.S. et al. Mental health and COVID-19 vaccine hesitancy among health-related university students: a cross-sectional multi-center study. Trop Med Health 53, 71 (2025). https://doi.org/10.1186/s41182-025-00751-3 [↩]
- Konstantinou, P., Georgiou, K., Kumar, N., Kyprianidou, M., Nicolaides, C., Karekla, M., & Kassianos, A. P. (2021). Transmission of vaccination attitudes and uptake based on social contagion theory; A scoping review. Vaccines, 9(6), 607. https://doi.org/10.3390/vaccines9 060607 [↩]